As an expert in the commercialization of early-stage technologies, especially in the life science and medical device industries, Supriya Munshaw, senior lecturer at the Johns Hopkins Carey Business School, has monitored news of the vaccine development process during the COVID-19 pandemic.
In the following conversation, Munshaw offers insights on the likely time frame for a coronavirus vaccine, the steps involved in developing one, the most promising candidates currently in the labs of biotech companies, and why, years after the MERS and SARS outbreaks, a coronavirus vaccine still has not been produced.

Image caption: Supriya Munshaw
Some U.S. government officials are talking about a COVID-19 vaccine being ready in a year to 18 months. And some experts say that's too soon, if it's going to be a safe vaccine. What do you think is a likely time frame?
A year to 18 months is very optimistic. Typically, a safe and effective vaccine will take anywhere from 10 to 15 years for development if one is starting from scratch. The good news here is that coronaviruses aren't novel, and there are groups that have already been working on such viruses for a while, especially since the MERS-CoV and SARS-CoV epidemics. So we are not starting from scratch, but even then 18 months is quite optimistic. Given the urgency of the situation, it is most likely that the manufacturer and the FDA will work together to balance the risks and benefits of the vaccine, such that the first vaccine we get may not be the most effective as long as it is safe. Since vaccines are given to healthy individuals, the safety requirements are quite high.
What steps are involved in developing a vaccine for COVID-19? What are the challenges and costs?
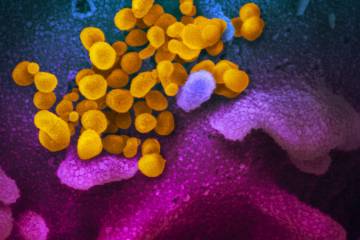
As the Centers for Disease Control and Prevention states on its website, vaccine development begins with an exploratory phase that involves identifying the appropriate antigens, or particles on the virus that can be used to elicit an immune response in the vaccine recipient. This is the basic research stage and can take anywhere from two to four years.
The next stage is pre-clinical studies, where the response to the identified antigen is observed in animals and in cell and tissue cultures, taking up to two years.
Next, we move on to the clinical trial stage, where in Phase I the vaccine candidate is tested in a small group of people (about 20 to 30) to ensure safety, followed by Phase II, where a larger group of individuals (typically hundreds to thousands) is tested for safety, dosage, and administration. Finally, in Phase III, the manufacturer tests the vaccine on thousands of people and looks for the incidence of disease in their large sample. It takes time to recruit people, find sites for clinical trials, and establish protocols. Once all that is done, these large vaccine trials can go on for anywhere from one to five years, because you are waiting to see if your vaccinated group has a lower incidence of disease than your placebo group.
Again, given the urgency of this situation, a surrogate endpoint may be used such that the effectiveness of the vaccine is measured in the type and length of immune response it can elicit. But even then, you're talking one to two years for this last phase alone. Also, one must remember that there is a high failure rate at each stage, so just because we found an antigen at the exploratory phase doesn't mean it will end up being a vaccine.
Another important aspect is scaling and manufacturing. Regulatory approval does not mean that enough vaccines can be manufactured quickly enough and then be available for the entire population. We often have flu vaccine shortages, even after planning those vaccines in advance.
Is it correct that a coronavirus vaccine has never been developed? If so, why wasn't one developed after the MERS and SARS outbreaks of the past two decades?
There are no vaccines to protect against any of the coronaviruses. But the research that was done during the previous epidemics may have shortened the exploratory and pre-clinical stages for the COVID-19 vaccine. That's why we already have vaccine candidates in Phase I. The MERS-CoV vaccine is still under development, but the disease is primarily contained to the Arab peninsula. And since SARS-CoV disappeared, a vaccine is no longer necessary.
Are there ways to speed up the vaccine development process through a coordinated effort between public and private entities?
The Coalition for Epidemic Preparedness Innovations is coordinating a majority of the efforts of vaccine discovery throughout the globe. It arranges funding, partnerships, and collaboration efforts among governments, pharmaceutical companies, and research organizations to speed up this process. For example, they brought together Moderna, the biotech company with a lead vaccine candidate in Phase I trials, and the National Institute of Allergy and Infectious Diseases to conduct the trial.
View this post on Instagram#JHUCarey faculty expert Supriya Munshaw shares insights into vaccine development. #Covid19
What are the most promising vaccine candidates right now?
Several companies are working on vaccine candidates. We have candidates from Moderna, Inovio, CanSino Biologics, and Shenzhen Genoimmune Medical Institute in the lead in Phase I trials. The others are in preclinical or exploratory stages. Interestingly, a trial is about to begin in Australia to test the effectiveness of the bacillus Calmette–Guérin vaccine—typically used to prevent tuberculosis—against COVID-19. We know this vaccine is already safe, so that's taken care of. It will be interesting to see if it is effective.
Do you see a coronavirus vaccination, once developed, becoming an annual occurrence, similar to influenza vaccinations?
It depends on how long the virus lasts and how fast it mutates. The SARS-CoV disappeared before a vaccine was ever developed. There are several hypotheses why this happened, but no one knows exactly why. The social distancing and isolation measures taken during that time probably played an important role in curbing the spread.
In terms of its mutation rate, influenza has lasted and has a very high mutation rate, meaning the virus changes rapidly, and several strains are often in circulation. So every year a vaccine is made based on predictions of the strains that will be around that year. Even then, influenza vaccines don't confer 100% protection because it is difficult to predict every single mutation.
Posted in Health, Science+Technology, Voices+Opinion
Tagged vaccines, q+a, coronavirus