From the bubonic plague of the 14th century to the Spanish flu outbreak in 1918, the repercussions and effects of pandemics have changed how societies function. Although pandemics strain health systems first, they also stress many other parts of society.
The Hub reached out to Alexandre White, an assistant professor of sociology and history of medicine at Johns Hopkins University, to learn more about the societal repercussions and consequences of past pandemics. This conversation has been edited for length and clarity.
How do international responses to the COVID-19 pandemic compare with those of previous pandemics?
That's a complicated question on a couple of levels. COVID-19, in a lot of ways, is a particularly effective disease at destabilizing health systems, as well as global economic processes. The fact that it can transmit asymptomatically and produce fairly mild symptoms in many of the cases means that its capacity to spread is quite high and it is putting a real strain on health systems around the world.
Since 1851, the threat of epidemic spread from particular diseases has been a critical concern for nations and the international community. The International Sanitary Conferences, which began in 1851, aimed to prevent the spread of infectious disease without disrupting trade and traffic. From the late 19th century through World War II, the ISC [oversaw the international response to] the spread of three diseases—plague, cholera, and yellow fever—until those responsibilities were transferred to what we now know as the World Health Organization.
The response by the WHO to COVID-19 was organized quite quickly. Since 2005, WHO regulations have established protocols and criteria for national health system readiness and also for what constitutes a "public health emergency of international concern," or PHEIC. WHO declared a PHEIC for COVID-19 at the end of January, which highlighted the severity of the threat. This was intended to aggressively mobilize international responses.
What we've actually seen in response to WHO's PHEIC declaration, particularly in the U.S. and the EU, has been a limited capacity for testing potential cases, which means that aspects of our treatment capacity are weakened.
The COVID-19 pandemic is frequently compared to the 1918 Spanish flu pandemic and the 2009 H1N1 outbreak. Are these fair comparisons?
I think that, biologically, comparing COVID-19 to previous flu outbreaks is useful because the process of epidemic spread can be similar. Like COVID-19, flus are often spread through droplets. The differences arise in the populations that are most at risk. We're still learning about the profile for those most at risk for COVID-19. Also, we have more effective diagnostic tools and biomedical responses now than we did in 1918, as well as increased capacity and knowledge in the medical sector. That puts us in a better position to confront this pandemic. However, in the absence of the pharmacological intervention, the practices of social distancing and quarantine initiatives might look similar to those of 1918.
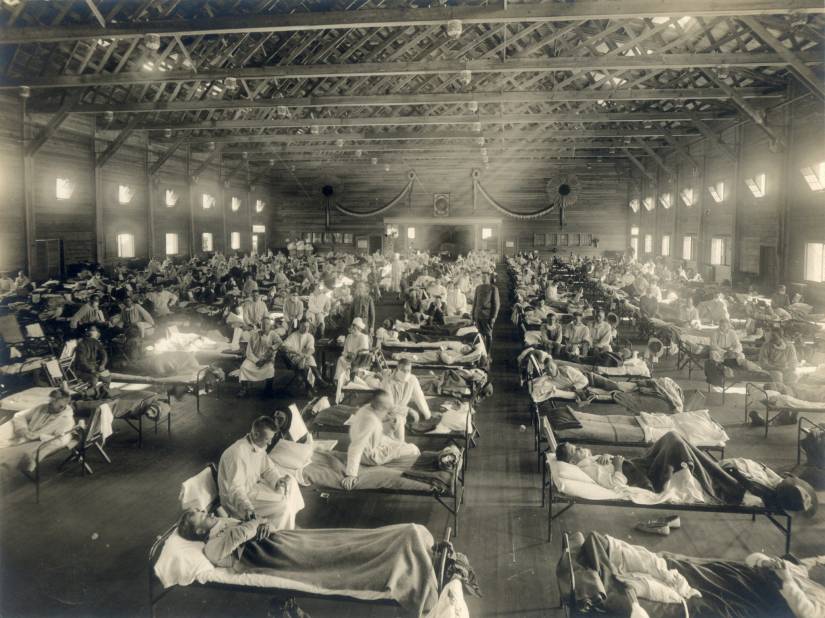
Image caption: Doctors and nurses tend to the sick in a converted infirmary at Fort Riley, Kansas, during the 1918 Spanish flu pandemic
Image credit: Associated Press / Wikimedia Commons
An epidemic that's largely been overlooked in comparison to this one is the most recent West African Ebola virus disease epidemic, as well as the recent Ebola epidemic in Democratic Republic of Congo. In these epidemics, aggressive, long-term social distancing measures were put in place in countries like Guinea, Liberia, and Sierra Leone. Although Ebola is biologically different in its method of contagion, we might still be able to look at the effective social distancing strategies carried out in West Africa for solutions to this current pandemic.
I hope we can recognize that social distancing measures are taken out of an abundance of care for one another, and we should be vigilant about how these practices protect the ones we love and the health workers confronting this disease.
There has been a lot of postulating on how public health measures, like social distancing, might change the nature of society. Historically, what are the lingering effects of global pandemics on societies?
In Cape Town in 1901, a plague epidemic produced a very aggressive racial segregated quarantine that, in many ways, became the precursor and blueprint for future segregated towns and communities in apartheid South Africa. It's a stark example of how racism and bigotry can drive very aggressive and oppressive responses against those most marginalized in a society.
Epidemics are crises. During crises, a lot of commonly held beliefs are questioned, and the status quo can be thrown into question, too. It's my hope that we can see how public health and socioeconomic disparities are widening as a result of the COVID-19 pandemic. Ideally, this will lead us to create better systems in the future.
Have there been any indications that the COVID-19 pandemic is exacerbating these inequalities?
Unfortunately, yes. The dangerous framing of this particular pandemic as a "Chinese virus" or the "Wuhan virus" leads to a great deal of stigma for anyone from China or of Asian descent. It leads to violence, harassment, hatred, and bigotry, as we've already seen. The ways in which this pandemic has exacerbated these particular practices of bigoted and racist ideology is not surprising during an epidemic, but it's a serious threat to effective health responses.
We've seen time and time again, in responses to HIV/AIDS in the 1980s or in responses internationally to bubonic plague from the early 1900s, that stigma and bigotry—especially when diseases become associated with certain people and communities—have the effect of creating a potentially vindictive public health response. We don't want to steer people who are sick away from the health care that they need because they're afraid they'll be persecuted or stigmatized for their illness.
The second aspect I'd want to touch on is how epidemics highlight inequality. We're starting to see it now in the high rates of unemployment that are stretching the capacities of our existing social welfare network in the United States. There have been very few national initiatives thus far for people who have been laid off from service work like employees at restaurants, in hospitality, and in recreation.
We are also seeing now how racial inequalities and existing health disparities are putting certain people at greater risk of severe symptoms and complications. These are the products of social inequality as much as epidemic dynamics. This needs to be addressed soon, and is emblematic of the declining social welfare network in the United States.
Posted in Health, Voices+Opinion, Politics+Society
Tagged sociology, history of medicine, q+a, coronavirus