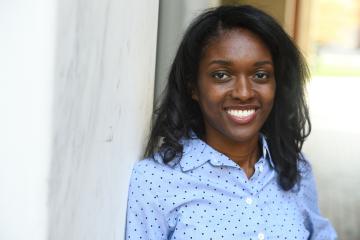
Muyinatu "Bisi" Bell conducts NIH-backed research to improve medical imaging so that every patient—regardless of skin color or body size—gets an early and accurate diagnosis.
"I aim to ensure that medical imaging technology serves all patients equally," said Bell, an associate professor in Johns Hopkins University's Department of Electrical and Computer Engineering at the Whiting School of Engineering. "By developing more precise imaging tools, we are doing more than advancing technology—we are changing how quality health care is delivered."
Video credit: Roy Henry / Johns Hopkins University
Named a winner of NIH's Trailblazer Award in 2018, Bell has spent the last decade refining photoacoustic imaging to provide detailed, real-time information about blood flow, oxygenation, and tissue composition without needing radiation or contrast agents. These capabilities make it an invaluable tool for surgeons and radiologists seeking to improve diagnostic accuracy and patient outcomes.
She led the creation of the world's first short-lag spatial coherence (SLSC) beamformer for ultrasound imaging—a key component that helps produce sharper, more reliable pictures. This advancement is important because conventional imaging techniques struggle to capture accurate details in patients with darker skin tones or larger body types due to differences in how light and sound waves interact with various tissues.
"NIH support has been immensely foundational toward enabling us to develop new solutions that work for everyone," said Bell, who has a joint appointment in the Department of Biomedical Engineering and directs the PULSE Lab.
Beyond improving diagnostic accuracy, Bell's innovations are also reshaping how surgical procedures are carried out. She pioneered the integration of photoacoustic imaging into the da Vinci surgical robot, making complex procedures safer by providing surgeons with a clearer picture of blood vessels, metal implants, and other structures during procedures.
"Surgeons rely heavily on imaging to navigate complex anatomical structures and avoid critical blood vessels and nerves," she said. "My work enhances intraoperative imaging, allowing surgeons to see in real time changes in tissue with great precision. This reduces the risk of complications, shortens recovery times, and improves overall patient outcomes."
Bell is also leveraging artificial intelligence to expand the potential of medical imaging. AI-powered algorithms can analyze vast amounts of imaging data to detect patterns and anomalies that may be invisible to the human eye. One application of this approach is using AI-enhanced imaging to detect COVID-19 in lung scans, helping doctors diagnose and monitor patients with greater speed and accuracy.
"We developed this automated detection tool to help doctors in emergency settings with high caseloads of patients who need to be diagnosed quickly and accurately, such as in the earlier stages of the pandemic," Bell said. "Potentially, we want to have small wireless devices that patients can wear at home to monitor the progression of COVID-19 and other respiratory diseases."
This technology could also be adapted into wearable patches for patients with conditions like pneumonia, allowing them to track fluid buildup in their lungs. By providing real-time monitoring, these devices could help doctors and patients manage treatment more effectively and adjust medications as needed.