A multidisciplinary team from the Bloomberg School of Public Health and the School of Medicine has found that organoids made from human brain cells, known as "mini-brains," can be infected by the SARS-CoV-2 virus, which causes COVID-19. Early reports have suggested that more than a third of COVID-19 patients show neurological symptoms, but until now it was not clear whether the virus infects human brain cells.
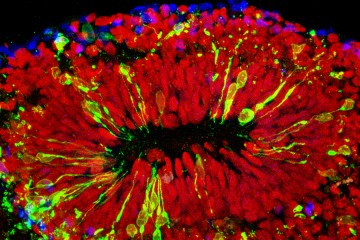
Through their use of tiny tissue cultures that simulate whole organs, the researchers have now demonstrated that certain human neurons express a receptor, ACE2, that the SARS-CoV-2 virus uses for entering the lungs—and possibly the brain. When the researchers—neurotoxicologists and virologists from the Bloomberg School and infectious disease specialists from the School of Medicine—introduced SARS-CoV-2 virus particles into a human "mini-brain" model, the team found what is believed to be the first evidence of infection by and replication of the pathogen.
The results were published online June 26 in the journal ALTEX: Alternatives to Animal Experimentation.
The human brain is well-shielded against many viruses, bacteria, and chemical agents by the blood-brain barrier. "Whether or not the SARS-CoV-2 virus passes this barrier has yet to be shown," notes senior author Thomas Hartung, chair for evidence-based toxicology at the Bloomberg School of Public Health. "However, it is known that severe inflammations, such as those observed in COVID-19 patients, make the barrier disintegrate."
The impermeability of the blood-brain barrier, he adds, also can present a problem for drug developers targeting the brain.
The impact of SARS-CoV-2 on the developing brain is another concern raised by the study. Other research from Paris Saclay University has shown that the virus crosses the placenta, and embryos lack the blood-brain barrier during early development, though the implications of this vulnerability are still unclear. "To be very clear," Hartung says, "we have no evidence that the virus produces developmental disorders."
However, the mini-brains contain from the very earliest stages the same ACE2 receptor that allows the virus to enter lung tissues. Therefore, Hartung says, the findings suggest that extra caution should be taken during pregnancy.
"This study is another important step in our understanding of how infection leads to symptoms, and where we might tackle the COVID-19 disease with drug treatment," says William Bishai, professor of medicine at the Johns Hopkins University School of Medicine, and leader of the infectious disease team for the study.
"There is no doubt that the virus infects neurons and multiplies" Hartung adds, "and now we have to find out what this means for patients and public health."
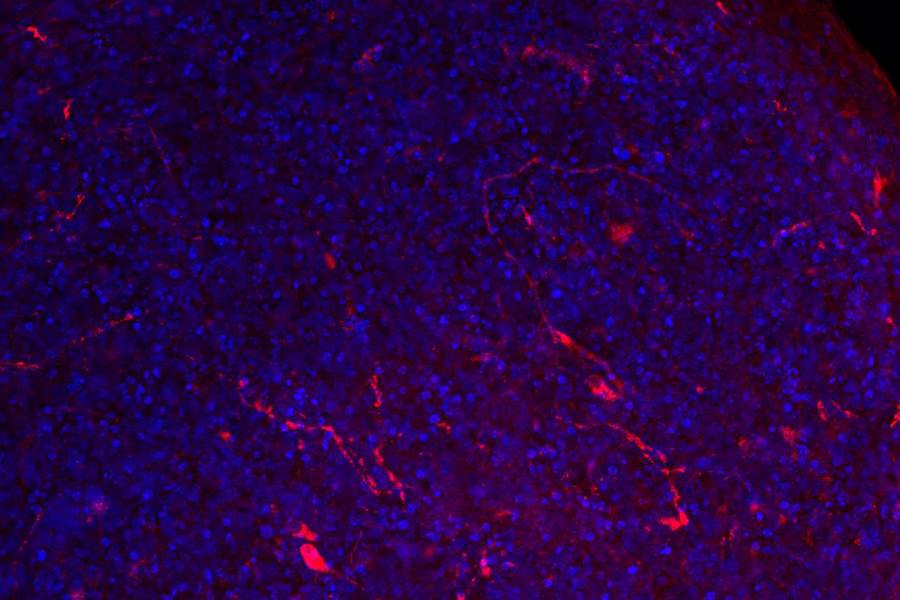
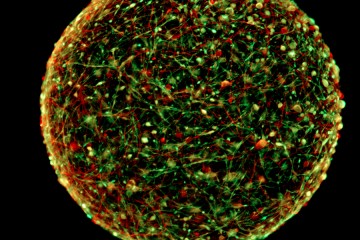
The human stem cell-derived "mini-brain" models—known as BrainSpheres—were developed at the Bloomberg School of Public Health four years ago. They were the first mass-produced, highly standardized organoids of their kind and have been used to model a number of diseases including infections by viruses such as Zika, dengue, and HIV.
Posted in Health, Science+Technology
Tagged neuroscience, coronavirus, covid-19, mini-brains