One of the more challenging aspects of the coronavirus pandemic has been the prevalence of asymptomatic cases, or people who are infected with the virus and can spread it to others but do not feel sick. In Iceland, where a broad testing effort resulted in 5% of the country's population being tested for COVID-19, a lab study suggests that as many as 50% of people who have the disease show no symptoms. A study conducted in Singapore showed that patients with COVID-19 were able to spread the disease without showing symptoms themselves.
To learn more about the issue of asymptomatic spread of COVID-19, the Hub reached out to Gigi Gronvall, an immunologist and senior scholar at the Johns Hopkins Center for Health Security and an associate professor at the Johns Hopkins Bloomberg School of Public Health. This conversation has been edited for length and clarity.
What are the implications of asymptomatic spread for the COVID-19 pandemic?
Asymptomatic spread has not been good news thus far. A growing body of results shows that people who are asymptomatic appear to have the same viral load as symptomatic cases. This means that, whether people have symptoms or not, they carry the same amount of virus inside them. This suggests that transmission is possible equally from both asymptomatic patients and noticeably sick patients.
To my knowledge, this is quite uncommon for a virus and is not a good sign. If you're able to transmit the virus while asymptomatic, it allows for a lot more community spread. For other viruses, you're not contagious until you have symptoms, so it's easier to screen for the disease and limit these chains of infection. COVID-19 is proving much harder to contain.
Why are we starting to hear that the novel coronavirus may have been circulating in the U.S. much earlier than previously thought?
Part of the reason these cases are coming to light now is due to the ongoing, combined challenges of insufficient testing and asymptomatic spread. Testing provides public health officials with situational awareness of the outbreak and the connections between those who might be carrying and spreading the virus, even if they don't feel sick. Being able to follow these chains of connections allows officials to follow the virus in real time, which is why testing is so crucial. One reason that we're now finding cases that occurred earlier than previously thought is that, if you don't have a test for a disease that's very new, like this coronavirus, it takes time to ramp up testing to necessary levels. Missing cases is one of the outcomes when it takes so long to do large-scale testing.
How can we effectively identify asymptomatic cases of COVID-19?
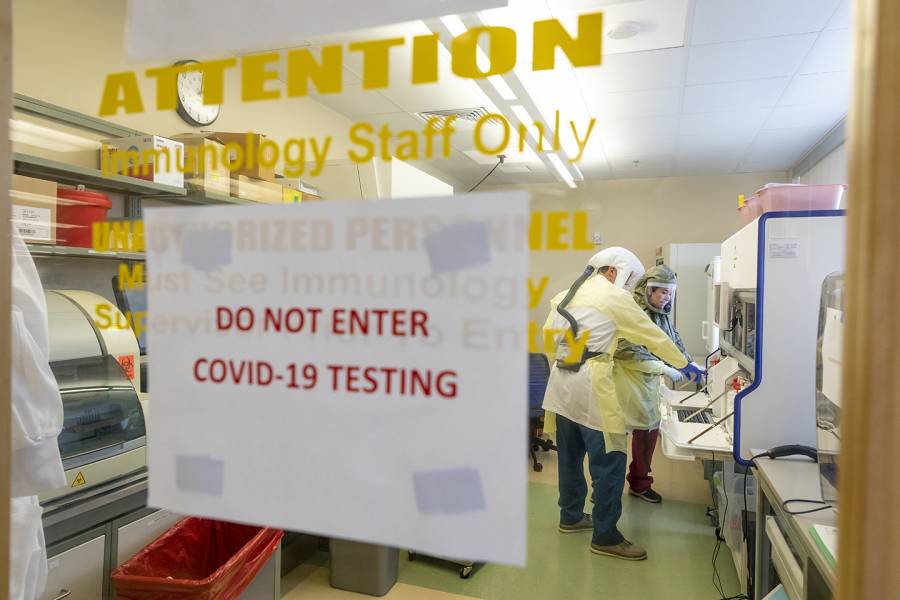
Current testing methods can detect asymptomatic cases. When you are infected with the coronavirus, the tests are pretty sensitive to any presence of the virus. The most common test at the moment is a PCR test, which looks for the presence of the virus's genetic material, and some of these are more sensitive than others. PCR tests are a way to amplify a small signal. It makes minicopies of the virus's genetic material—so you take the sample from a patient, and if there's a trace of the virus, you're able to find these small pieces of it, even if it's present in very low quantities. The test results take about two to four hours to complete and you need to use a laboratory to do so.
There are other useful tests, including a rapid antigen test. The rapid antigen test is like a test for strep throat and would take about 15 minutes for a result. The rapid antigen test looks for the virus's proteins, usually in a saliva sample, and while it's not as sensitive as PCR, it's fast and can be done anywhere. There are different tests for different purposes, and while rapid tests aren't as sensitive, they are useful. Testing of all kinds is a good thing, and we need to see a lot more of it.
The best test really depends on the environment—it's OK to have different kinds of tests and different makers, but not all of them are going to serve the same function for the same purpose. A rapid test is great to screen lots of people, but if you get a negative result you might need to follow it up with a more in-depth test to see if someone has an active COVID-19 infection that wasn't picked up by the test. Because of asymptomatic spread of the coronavirus, we're going to need a lot more testing and have public health officials actively look for cases. Then, when cases are identified, individuals who came into contact with them must be isolated, to break the chains of transmission. This is what's often referred to as contact tracing.
Given concerns about asymptomatic spread, how can governments protect public health and also plan for the eventual easing of social distancing measures?
There are numerous tools available to both governments and local communities, as well as individuals, though none of them are perfect. Unfortunately, this is going to have to be an altered way of life for all of us until we can get to full coverage from a vaccine. First, we need widespread viral testing to determine who is currently infected with COVID-19. Another tool is serology testing, which tests to see if people have antibodies to fight the virus, which would potentially give them a level of protection and immunity. Another tool is training a large contingent of public health officials to work as contact tracers to break the chains of infections.
There are also nonpharmaceutical interventions that we've all become familiar with, like wearing masks, staggering hours when businesses are open and people are together, and also limiting gatherings. All of these are not the same as getting back to "normal," but all of these approaches help to maintain public health, to limit spread, and to keep us going until the solution—a vaccine—is available.
There are over 160 different vaccines and therapies being tested at the moment. We have to hope that, with so many "shots on goal" at a vaccine or treatment, maybe a few will be successful. It's not ideal, but this is how things are going to have to be to contain the virus spread.
What is an "immunity passport" and does it come with unintended consequences?
We're learning a lot about individuals who have had COVID-19, and one idea has been to use a serology or antibody test to provide an "immunity passport" to free them from the constraints of physical distancing. To be clear, this would not be a good idea. Notably, we don't understand yet the durability of immunity to COVID-19, and due to the risks of false positives and false negatives from the test, you might wrongly categorize someone who does not in fact have immunity. It's very problematic to allow a certain, select group to go outside and forgo physical distancing measures.
We're also concerned about the idea of perverse incentives. If someone isn't allowed to work unless they're immune to COVID-19, there's the potential for fraud, or for people to fake their immunity, which would put them and others at risk. There's also a chance that, to try to achieve immunity, people deliberately try to get the disease, which is also deeply hazardous. This is why public health officials have advocated for using a suite of tools to limit spread until there's a vaccine. Testing is important, but the idea that you're immune can't be the only criterion for loosening restrictions. We need other public health interventions, and it would be bad news if we created incentives where people need to get sick to keep their jobs.
I'm an optimistic person and I've been thrilled by how fast the scientific community has moved to learn about virus, to collaborate to understand and treat the virus, and to ultimately get to a vaccine. There are so many brilliant people working toward that goal, but until we reach it, we have to endure during this in-between time that we're in.
Posted in Health, Politics+Society
Tagged epidemiology, immunology, coronavirus, covid-19