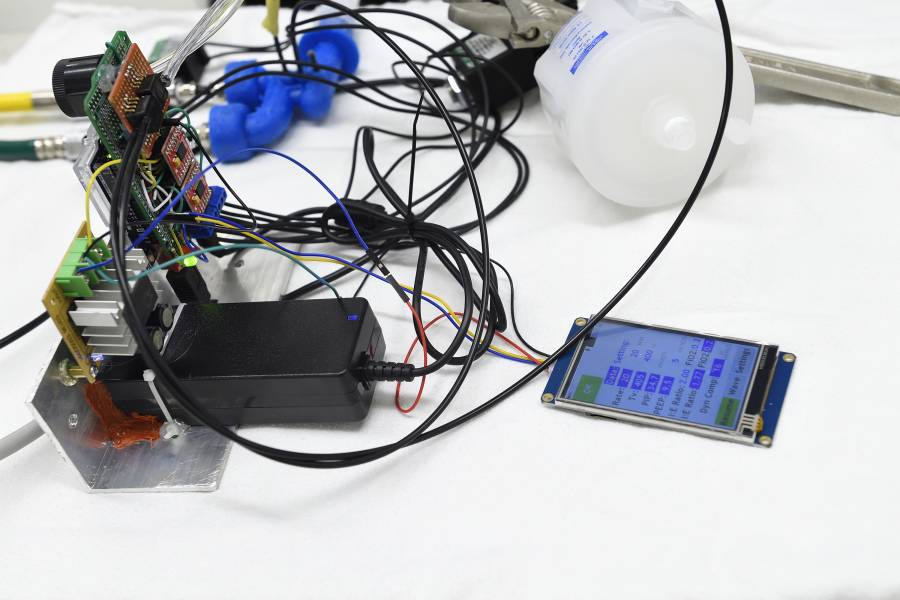
A team of Johns Hopkins engineers has developed a prototype for a pumpless ventilator that can run for 24 hours on a single 12-volt battery. Designed to operate on pressurized air and oxygen lines already available in hospitals or from simple pressurized air and gas sources in the field, the device has fewer moving parts than traditional ventilators and can be manufactured quickly and relatively inexpensively—factors especially crucial during the current COVID-19 pandemic.
The team is now testing its prototype in the Johns Hopkins Medicine Simulation Center.
"We went with a pumpless design because of its simplicity—fewer moving parts," says Nick Keim, deputy director of the Johns Hopkins School of Engineering's Energetics Research Group and leader of the team developing the prototype. "By not having a pump, we push that part of the problem outside of the ventilator itself, and the design and manufacturing for the parts that are specific to the patient get simpler. These ventilators can share infrastructure that already exists in hospitals. Even outside of hospitals, it will be relatively easy to distribute pressurized oxygen from a liquid oxygen truck to patients."
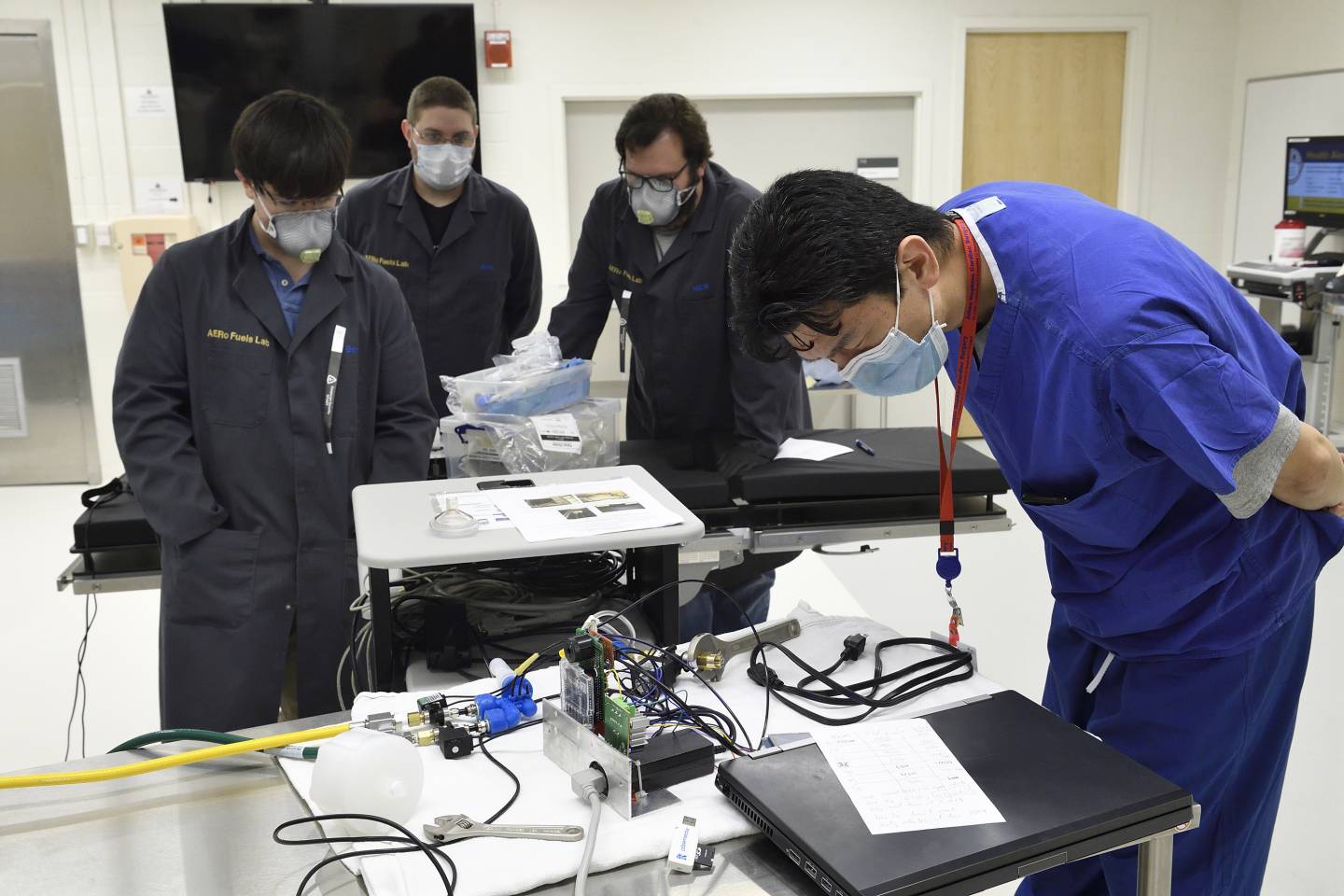
Image caption: Researchers (from left) Ben Hill-Lam, Alex Bishop, Nick Keim, and Bo Soo Kim test the pumpless ventilator in the Johns Hopkins Medical Simulation Center
Image credit: Will Kirk / Johns Hopkins University
The parts for the prototype were 3D printed in Keim's AERo Fuels Laboratory, where rocket fuels are tested for thermal stability. The concept for the device's precise control of the flow of gases was born from the lab's expertise in fluid dynamics.
The team's design includes three actively controlled valves, two sensors, and two mechanical safety valves for backup to keep the patient safe in case the main valves fail. The rest of the design depends on a control algorithm that ensures all critical requirements for medical ventilation are met. The team is also developing software to monitor multiple ventilators from a central location, such as a nurses' station.
Bo Kim, assistant professor of medicine at the Johns Hopkins School of Medicine, is providing Keim's team with medical expertise and feedback. He says the new design is unique and promising.
"Conventional ventilators are always preferred, but if this design works, it could provide an alternative in situations where there is a shortage and it is absolutely necessary for a patient to be on a vent," he says.
The prototype is assembled using components that can be quickly mass produced. But before the ventilator can enter production, there are a few challenges to surmount, such as determining the fastest way to manufacture the units.
"Right now our primary design is 3D printed, but at the end of the day, 3D printing is fast for prototyping but slow for mass manufacture," Keim says.

Image credit: Will Kirk / Johns Hopkins University
Personnel in the Instrument Development Group at the Johns Hopkins Krieger School of Arts and Sciences helped transform the design into one that can instead be created using injection molds. Although the upfront costs of using injection molds are higher, Keim says that when amortized over 10,000 units, the process becomes significantly less expensive than 3D printing would be. For example, a part that would cost $50 when 3D printed would cost about $10 when produced at scale through injection molding. In addition, the speed of manufacturing the parts with injection molding will be much faster, he says.
The team is also working around supply shortages, such as for a type of electromagnet needed to make the valves.
"We've been designing, printing, assembling, ordering, and reassembling and testing pretty much nonstop," Keim says. "Logistics have become a challenge recently as well, we've only been at it for two weeks, but it is already getting more difficult to order the parts we need to iterate on the design."
Keim's goal is to have 10,000 ventilators made from his design over the next three months.
"We're talking about potentially lifesaving devices. If we don't deliver, then they won't exist; and they have to work, and work well, for weeks on end," Keim says. "I'm not under any delusion that this is the only option or that we're the only team working it, but the reality is that even if all the teams were able to come up with 10,000 ventilators that meet doctors' and patients' needs, there still probably won't be enough to go around."
Posted in Health, Science+Technology
Tagged 3-d printing, coronavirus, covid-19