- Name
- Barbara Benham
- bbenham1@jhu.edu
- Name
- Robin Scullin
- rsculli@jhu.edu
With a vaccine for COVID-19 still a long way from being realized, Johns Hopkins immunologist Arturo Casadevall is working to revive a century-old blood-derived treatment for use in the United States in hopes of slowing the spread of the disease.
With the right pieces in place, the treatment could be set up at Johns Hopkins University in Baltimore within a matter of weeks, Casadevall says.
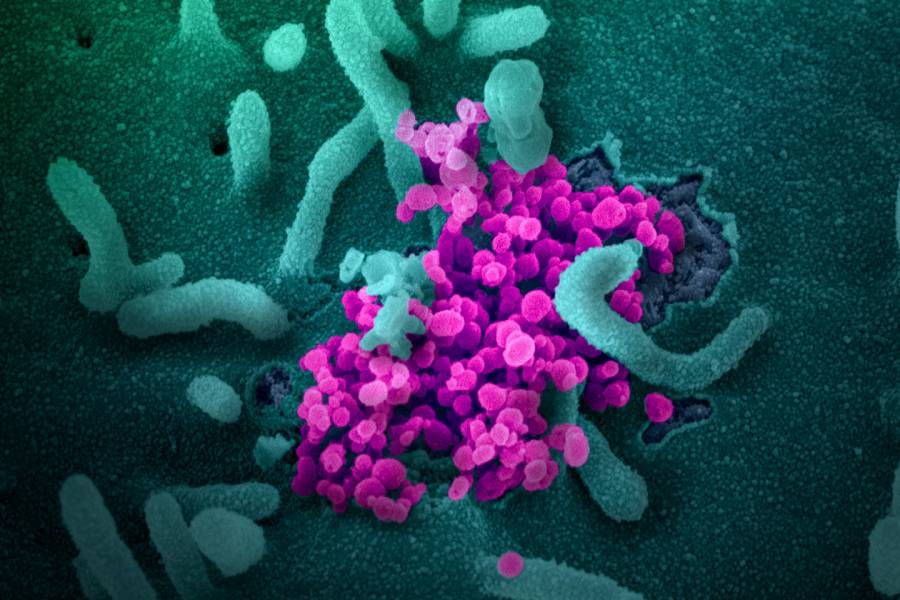
The technique uses antibodies from the blood plasma or serum of people who have recovered from COVID-19 infection to boost the immunity of newly infected patients and those at risk of contracting the disease. These antibodies contained in the blood's serum have the ability to bind to and neutralize SARS-CoV-2, the virus that causes COVID-19. Casadevall—a Bloomberg Distinguished Professor of molecular microbiology and immunology and infectious diseases at the Johns Hopkins Bloomberg School of Public Health and School of Medicine—published a paper on the proposal today in The Journal of Clinical Investigation.
"Deployment of this option requires no research or development," he says. "It could be deployed within a couple of weeks since it relies on standard blood-banking practices."
In this case, physicians would ask patients who recover from COVID-19 to donate their blood, from which sera would be isolated. After processing the serum and removing other toxins or trace illnesses, it can be injected into sick patients and those at risk of contracting the disease. The procedure for isolating serum or plasma is a long-established technology that can be performed using equipment normally found in hospitals and blood-banking facilities, and recent advances make it as safe as a blood transfusion, Casadevall says.
Experts around the U.S. are rushing to implement the treatment in several different areas, including New York City, Casadevall says. Doctors in Shanghai have already used the plasma therapy with newly infected coronavirus patients in China and have reported promising early results. Japan's largest drugmaker, Takeda Pharmaceuticals, has also begun testing the therapy.
The Johns Hopkins Research Team has put initial funding toward Casadevall's project, to purchase equipment and set up an operation in Baltimore. Casadevall and his team are working now with state and federal officials to try to secure more resources.
The medical concept—known as "convalescent plasma" or "convalescent sera"—dates back to the early 20th century, and was used successfully in the past to counter epidemics including mumps and the measles. In a recent Wall Street Journal op-ed, Casadevall points to a notable case preventing a measles outbreak at a U.S. prep school in 1934.
Experts say a challenge of the technique is that precise timing is important in order to maximize the boost to a patient's immunity. The treatment is not envisioned as a panacea to treating coronavirus, but a temporary measure that could help until stronger options such as vaccines are available.
"It's all doable—but to get it done it requires effort organization, resources… and people who have recovered from the disease who can donate the blood," Casadevall says. He adds that many people have stepped up to the plate at Hopkins and are already working to put this system in place.
Casadevall says he believes the solution "could do a lot locally" in the Baltimore region. He also noted that Johns Hopkins could become the Investigational New Drug (IND) center in the U.S. for this treatment, helping to administer it across states.
Learning more about how to use the sera most effectively will require further clinical studies. "We will learn new science from this calamity," Casadevall says.
Posted in Health, Voices+Opinion
Tagged bloomberg distinguished professorships, arturo casadevall, coronavirus