Breast cancer is deadliest when it metastasizes, or spreads. The five-year survival rate for patients with breast cancer that's confined to the breast is 99%, according to the American Cancer Society, but that rate drops to just 27% once the cancer spreads to a distant part of the body.
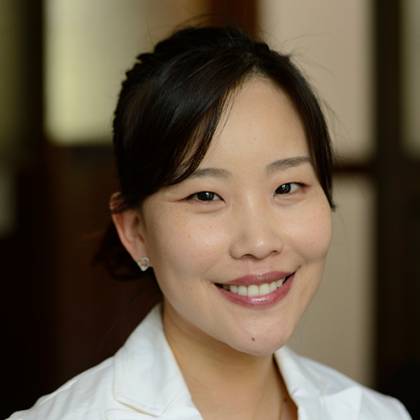
Image caption: SJ Claire Hur
Image credit: Will Kirk / Johns Hopkins University
Johns Hopkins mechanical engineer SJ Claire Hur is embarking on an effort to develop a microfluidics device that can collect and genetically modify tumor cells from the blood samples of metastatic breast cancer patients. These purified and modified cells will enable scientists to monitor the patient's cancer progression in a lab, and to develop and test personalized treatment plans. These models may even eliminate the need for some cancer patients to undergo frequent invasive biopsies or surgeries, Hur said. She was recently awarded a $450,000 Career Catalyst Research Grant from the Susan G. Komen Foundation to support her work.
"If we have an efficient way to culture collected circulating tumor cells in the lab, researchers can perform numerous biological experiments and functional tests directly on patient-derived tumor cells," Hur said in an interview with the Department of Mechanical Engineering last month. "This will help identify the most effective therapeutic option for the patients."
The Hub reached out to Hur for more information on this cell culture project and for insights into what mechanical engineering can bring to the field of cancer research.
How does your work fit into the wide landscape of breast cancer research as a whole?
We're developing a project aimed at helping individual patients who haven't yet identified appropriate therapeutic options for their condition. Everyone responds differently to treatment at later stages of breast cancer, so if the cancer becomes metastatic, patients have fewer treatment options available to them. Our goal is to create a device that assesses individual cancer specimens more easily and more accurately so oncologists can test different therapeutic strategies and find the right one at the right time when the patient needs it.
How does your device work?
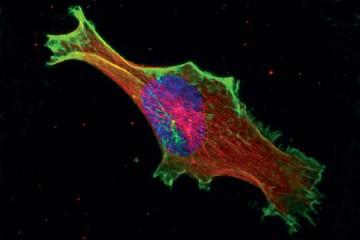
It collects circulating tumor cells from a small amount of the patient's blood—typically about 10 milliliters—and delivers genes to those purified cells to enable them to grow in a lab. It allows researchers to create an ex vivo tumor model—which means it uses the patient's sample but is grown outside the body—that will replicate what's happening inside the patient's body. Oncologists can then test different treatment options and identify the best one for that patient.
How does a microfluidics approach help breast cancer patients?
Basically, if close monitoring of breast cancer is important, then the strategies for routine assessment have to be non-invasive. It's not sustainable for patients to undergo routine surgeries or biopsies. So our target approach involves routine blood draws, which are less invasive than other approaches.
What drew you to this type of work?
During the second year of my PhD, my cousin died of cancer at age 41. He was a doctor, and the first person to offer me a contract as an engineer. He used to tell me that after I became an engineer he wanted me to build devices for his work. He was my friend and my role model, so I really struggled after he died to find meaning in my work. But around that time I met my PhD adviser, who was working on a cancer project, and we developed tiny instruments that could assess a patient's specimen more accurately. So the research tied in really well to the things that became important to me after my cousin died.
So it's personal.
Yes, really personal.
What are the advantages of bringing a mechanical engineering perspective to cancer research?
Well, when people ask me what I do, I usually say I'm a tool developer. I think mechanical engineers are people who are great at creating tools that don't exist yet. And a lot of recent medical advances involve the development of new technology. We knew about DNA without modern technology, for example, but without that technology you wouldn't be able to sequence DNA to the extent we are now. And now we're using it for advanced diagnostics and other DNA therapies. So I believe tools have the power to contribute to and advance medicine.
Posted in Science+Technology, Voices+Opinion
Tagged mechanical engineering, breast cancer, microfluidics, q+a