- Name
- Rachel Butch
- rbutch1@jhmi.edu
- Office phone
- 410-955-8665
- Name
- Vanessa Wasta
- wasta@jhmi.edu
- Office phone
- 410-955-8236
A new study from the Johns Hopkins University School of Medicine shows that selectively removing senescent cells—cells that no longer divide—from brains with a form of Alzheimer's disease can reduce brain damage and inflammation and slow the pace of cognitive decline. These findings, say researchers, add to evidence that senescent cells contribute to the damage caused by Alzheimer's disease.
"Our results show that eliminating these cells may be a viable route to treat Alzheimer's disease in humans," says Mark Mattson, a professor of neuroscience at the School of Medicine and a senior investigator in the Laboratory of Neurosciences at the National Institute on Aging.
A report on the work was published April 1 in Nature Neuroscience.
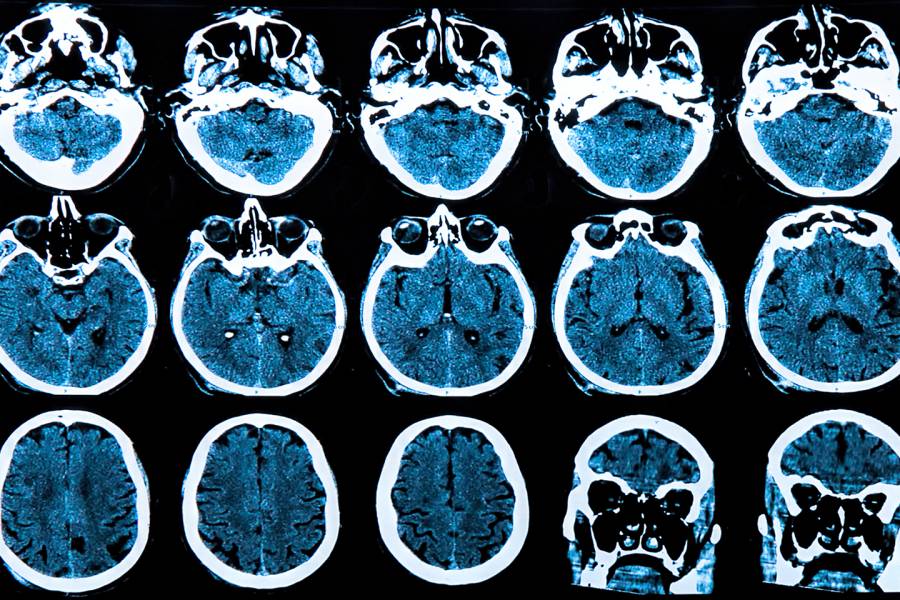
Alzheimer's disease is an age-related degenerative disease of the brain that affects an estimated 5.8 million Americans. The disorder—the most common cause of age-related dementia—is marked by the aggregation of amyloid proteins, which can kill off surrounding neurons. The areas of amyloid accumulation and associated nerve cell death, called plaques, are a hallmark of the disease. To date there are no known successful treatments for the disease, and as these plaques begin to form, patients experience progressive memory loss, learning impairment and, in later stages, delusions and paranoia.
Researchers have found that a specific brain cell type, called oligodendrocyte progenitor cells, appears in high numbers near plaques. In a healthy brain, these progenitor cells develop into cells that support nerve cells, wrapping them in a protective layer that heals injury and removes waste. The environment created by the amyloid proteins causes these progenitors to stop dividing and conducting their normal functions. In diseases such as Alzheimer's, the oligodendrocytes progenitor cells instead send out inflammatory signals that contribute more damage to the surrounding brain tissue.
"We believe the amyloid is damaging the neurons, and although the oligodendrocytes move in to repair them, for some reason the amyloid causes them to senesce rather than complete their job," Mattson says.
The researchers suspected that if they could selectively remove these malfunctioning senescent oligodendrocyte progenitor cells, they could slow Alzheimer's disease progression.
The researchers tested the concept in mice that were genetically engineered to have some of the characteristics of Alzheimer's disease, such as aggregated amyloid plaques. To remove the senescent cells, the researchers devised a treatment with a mixture of two U.S. Food and Drug Administration-approved drugs: dasatinib and quercetin. Dasatinib was originally developed as an anti-cancer drug, and quercetin is a compound found in many fruits and vegetables. The drug combination was proven as an effective way to eliminate senescent cells in previous studies of other diseases.
The researchers administered the drugs to groups of the Alzheimer's mice for nine days, then examined sections of the brains for signs of damage and the presence of senescent oligodendrocyte progenitor cells.
They report that the mice treated with the drugs had approximately the same amount of amyloid plaques as mice that received no treatment. However, the researchers say they found that the number of senescent cells present around these plaques was reduced by more than 90 percent in mice treated with the drug combination.
They also found that the drugs caused the senescent oligodendrocyte progenitor cells to die off. Together, these results show that the dasatinib and quercetin treatment effectively eliminated senescent oligodendrocyte progenitor cells.
The researchers next tested whether the physical benefits of the dasatinib and quercetin treatment could protect the mice against the cognitive decline associated with Alzheimer's disease. To do that, the researchers periodically evaluated the mice's cognitive function by observing how they navigated mazes.
They found that after 11 weeks, control mice who got no drug treatment took twice as long to solve the maze as their counterparts treated with dasatinib and quercetin.
After 11 weeks, the researchers again analyzed the brains of the mice and found 50 percent less inflammation in mice treated with dasatinib and quercetin, compared with non-treated mice. The researchers say these results show that eliminating senescent cells from the brains of affected mice protected cognitive function and reduced inflammation linked to Alzheimer's disease-like plaques.
Cellular senescence is an emerging area of interest in studies of age-related disease such as Alzheimer's, says Mattson. It has been most extensively studied in peripheral tissues, such as skin, where older cells are rapidly replaced by new ones. In these tissues, senescent cells accumulate as a normal part of aging, causing some of the well-known signs of aging skin, including wrinkles, stiffness, and fragility.
Mattson cautions that mice genetically engineered to have Alzheimer's symptoms and characteristics do not directly mimic the biological processes of the human condition. For example, mouse brain cells do not die as amyloid plaques form, while human brain cells do.
Posted in Health
Tagged brain science, neuroscience, alzheimer's disease, cognitive science