Studying a new type of lab-grown brain—made with technology first suggested by three high school students—Johns Hopkins researchers have confirmed a key process by which Zika virus causes microcephaly and other damage in fetal brains.
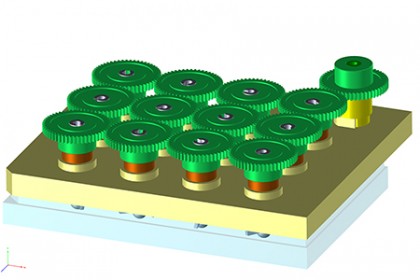
Image caption: The SpinΩ bioreactor (green) used to create the conditions for mini-brains to grow. At bottom is a commercially available 12-well lab dish.
Image credit: Johns Hopkins Medicine
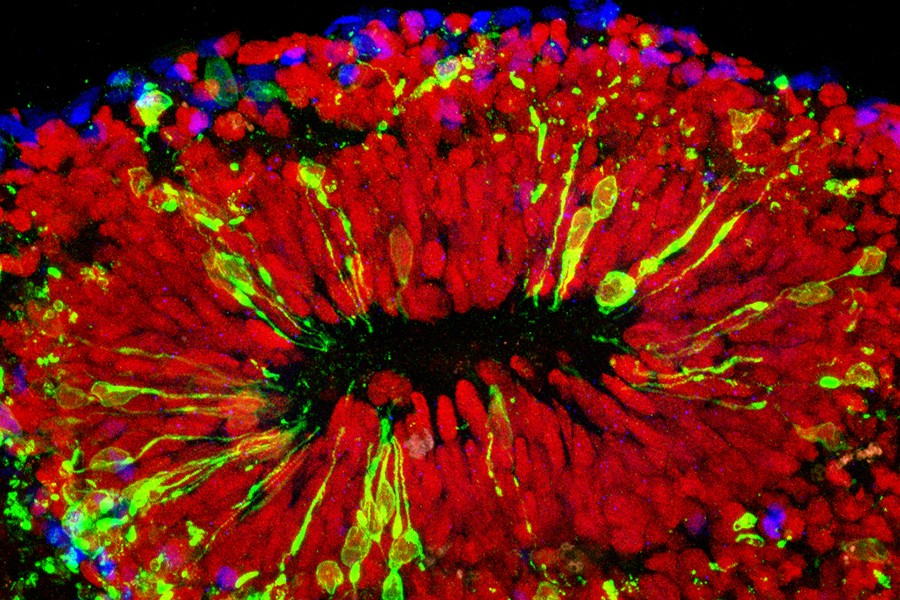
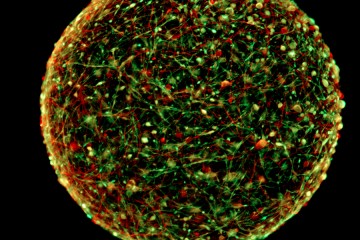
The scientists confirmed that Zika infects specialized stem cells that build the brain's outer layer, the cortex. A report on the research appears online today in the journal Cell. The researchers say the mini-brains used in the experiment are truer to life and more cost-effective than similar research models.
"We have been working for three years to develop a better research model of brain development, and it's fortunate we can now use this one to shed light on the major public health crisis posed by Zika infections," says Hongjun Song, professor of neurology and neuroscience at the Johns Hopkins University School of Medicine's Institute for Cell Engineering. "This more realistic, 3-D model confirms what we suspected based on what we saw in a two-dimensional cell culture: that Zika causes microcephaly—abnormally small brains and heads—mainly by attacking the neural progenitor cells that build the brain and turning them into virus factories."
Existing techniques for creating and working with mini-brains were limited because of the organ's complexity, Song says. The brains grow in comparatively large bioreactors and require chemical growth factors that guide the tissue to organize like a real brain, making growing and working with the mini-brains expensive.
Song and his wife and research partner, Guo-li Ming found a way to improve the bioreactors from an unexpected source: their son and two other high school students, from New York and Texas, who spent a summer working in the lab. The students had worked with 3-D printers and thought they could be the key to producing a better bioreactor, one that would fit over commonly used 12-well laboratory plates and spin the liquid and cells inside at just the right speed to allow the cells to form brains.
Also see
Of course, it wasn't that simple, Song says. Graduate student Xuyu Qian and postdoctoral fellow Ha Nam Nguyen spent years determining factors such as what that optimum spin speed was, as well as which chemicals and growth factors should be added at what times to yield the desired result.
The group has so far used the new bioreactor, dubbed SpinΩ, to make three types of mini-brains mimicking the front, middle, and back of a human brain. They used the forebrain, the first mini-brain with the six layers of brain cell types found in the human cortex, for the current study on Zika.
"One thing the mini-brains allowed us to do was to model the effects of Zika virus exposure during different stages of pregnancy," says Ming, who is a professor of neurology, neuroscience, and psychiatry and behavioral sciences at the Johns Hopkins School of Medicine. "If infection occurred very early in development, the virus mostly infected the mini-brains' neural progenitor cells, and the effects were very severe. After a while, the mini-brains would stop growing and disintegrate. At a later stage, mimicking the second trimester, Zika still preferentially infected neural progenitor cells, but it also affected some neurons. Growth was slower, and the cortex was thinner than in non-infected brains."
These different effects correspond to what clinicians have seen in infants born to women who contracted Zika during pregnancy, as well as miscarriages, she notes, namely that the earlier in pregnancy Zika infection occurs, the more severe its effects. The research group's next step will be to test drugs that are already FDA-approved for other conditions on the mini-brains to see whether one might provide some protection against Zika.
The team will include the 3-D printing files for SpinΩ in the new paper so that researchers anywhere can print their own bioreactors with just a few hundred dollars in materials.
Song says one possible future use for the technology could be to grow so-called dopaminergic neurons to replace those that die off in patients with Parkinson's disease.
"This is the next frontier of stem cell biology," he says.
Other authors on the paper are Mingxi M. Song of River Hill High School in Clarksville, Maryland; Christopher Hadiono of Byram Hills High School in Armonk, New York; William Jeang of Clear Lake High School in Houston, Texas; Sarah C. Ogden, Christy Hammack and Hengli Tang of Florida State University; Bing Yao, Li Lin, Yujing Li, Hao Wu and Peng Jin of Emory University; Gregory Hamersky and Brady J. Maher of the Lieber Institute for Brain Development; Fadi Jacob, Chun Zhong, Ki-jun Yoon, Jai Thakor, Daniel Berg, Ce Zhang, Eunchai Kang, Michael Chickering, David Naeun Zhexing Wen and Kimberly M. Christian of The Johns Hopkins University; Cheng-Ying Ho of George Washington University; and Pei-Yong Shi of the University of Texas Medical Branch.
Posted in Health, Science+Technology
Tagged epidemiology, neuroscience, zika virus