"We're at the start of what's looking like it will be a severe pandemic."
Tom Inglesby uttered these words to a group of international leaders in a New York City hotel meeting room on October 18, 2019, roughly two months before the first person in Wuhan, China, fell sick from a mysterious respiratory illness.
Inglesby, the director of the Johns Hopkins Center for Health Security, was not prognosticating on that fall day. He was playing a role in Event 201, a pandemic exercise the CHS created in partnership with the World Economic Forum and the Bill & Melinda Gates Foundation. The leaders Inglesby addressed—representatives from NBCUniversal, UPS, and Johnson & Johnson, as well as international public health leaders—were acting as the members of a high-level pandemic response team convened to address the disaster.
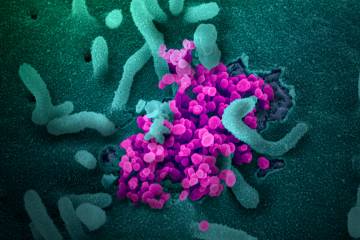
Event 201 was a work of imagination, a simulation or "tabletop exercise" as it's known in the field. But it was designed to feel terrifyingly real. At the beginning of the exercise, a "GNN-TV" special report informed participants that the source of the outbreak was a novel coronavirus that started in pigs in Brazil, then jumped to farmers, then spread globally, causing a respiratory illness with symptoms ranging from mild flu-like signs to severe pneumonia. Three months into the outbreak, there were nearly 30,000 cases and 2,000 deaths worldwide.
Over the next several hours, intermittent mock newscasts served up one crisis after another. The pandemic team did its best to grapple with the challenges. But the gaps in public health preparedness were too great to overcome. At the end of the exercise the team learned that, after 18 months, the pandemic had caused 65 million deaths and a devastating worldwide economic crisis. "Are there things we could have done in the five to 10 years leading up to the pandemic that would have lessened the catastrophic consequences?" a commentator asked in the final video. The point of Event 201 was to ensure everyone in the room answered yes.
In early January, the CHS issued a call to action based on the vulnerabilities Event 201 had dramatically revealed. To lessen the catastrophic consequences of a future pandemic, governments, industries, and international organizations needed to work together to increase stockpiles of medicine and protective equipment, create transportation and trade systems to distribute critical resources, bolster vaccine development and production, and combat mis- and disinformation, among other actions.
But the future arrived too quickly. By the time CHS published its recommendations on January 17, COVID-19 was already spreading from China throughout the world. The first case in the United States was diagnosed on January 21. The time for raising awareness and motivating action had passed. The CHS experts shifted to response and recovery, using their expertise to advise officials, educate the public, and recommend health and policy measures, all the while experiencing a surreal sense of déjà vu that the pandemic they'd simulated was eerily similar to reality.
When D.A. Henderson, legendary Hopkins doctor, epidemiologist, and leader of the international effort to eradicate smallpox, founded the Center for Health Security in 1998, the focus was on protecting the public from the threat of bioterrorism. CHS still deals with deliberate biological threats, but given we're in an age of epidemics—evidenced by SARS in 2003, H1N1 in 2009, and Ebola in 2013–16—the center has expanded its focus to include all manner of health disasters. Among its nearly 40 experts are epidemiologists, medical doctors, immunologists, infectious disease specialists, biologists, disaster preparedness experts, and economic modelers. Nearly all have contributed to the COVID-19 response effort.
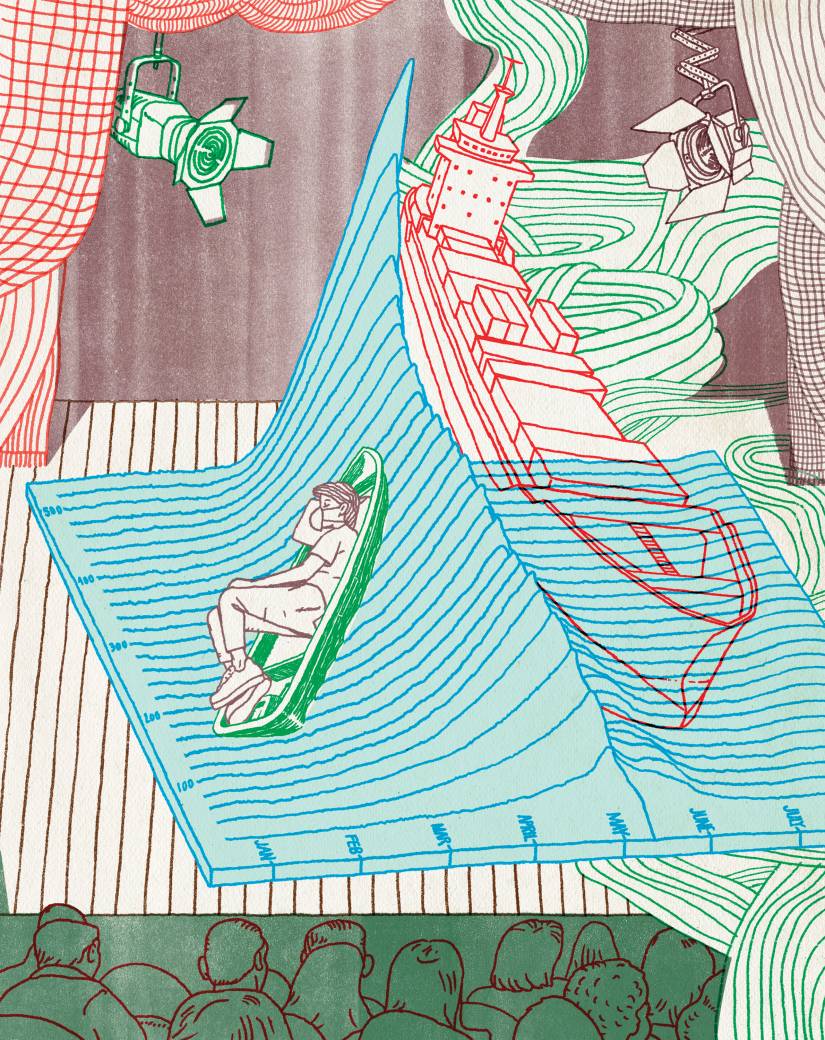
Image credit: Jeffrey Decoster
On January 2, CHS analyst Matthew Shearer first posted about the "mysterious illness in Wuhan" on Outbreak Observatory, a center project that studies worldwide response to outbreaks. Shearer, a former Navy anti-terrorism force protection officer who joined the center in 2015, said the post was meant to put rumors about the illness in context, particularly the rumor that it was SARS-related. Shearer was part of the core planning team for Event 201, and in the months that followed he would remark again and again about the strangeness of seeing scenarios they included in the exercise for "interesting conversation" actually happening in real life. But on January 2, he had no inkling we were on the verge of a pandemic.
Then, over the next three weeks, three pieces of information coming out of China set off a series of alarm bells, says Inglesby, Med '96 (HS), '96 (PGF), '99 (PGF). This illness was caused by a coronavirus, its reproductive rate appeared to be higher than that of influenza, and health care workers were getting ill and dying. CHS experts sprang into action, gathering and analyzing data, holding daily meetings, and urging leaders at all levels of government to plan for the possibility of a global outbreak.
In February, Inglesby, an international leader in pandemics and emerging infectious disease, met with Maryland's Deputy Secretary for Public Health Services, Fran Phillips, to communicate that "there was absolutely no time to waste in taking radical steps to prepare," Phillips says. At that meeting, Phillips says they discussed what then seemed like surreal responses: closing schools and businesses, imposing social distancing measures, and undertaking intense planning for a medical surge. She left convinced Maryland Gov. Larry Hogan would benefit from Inglesby's expertise, and Phillips soon became a charter member of the state's Coronavirus Task Force that meets by phone twice weekly with the governor.
"The governor has repeatedly ascribed the bold and early preventive actions that Maryland has taken to flatten the curve to the advice of his Coronavirus Task Force," says Phillips, an associate in the Department of Health Policy and Management who first worked with Inglesby on the H1N1 crisis in 2009. "On the frequent Coronavirus Task Force calls, Gov. Hogan consistently seeks out Tom's views. The governor clearly has great confidence in Tom's reasoned straight-talk perspective."
Along with many CHS experts, Inglesby spends much of his time advising officials, talking to reporters, appearing on national TV and radio—the CHS media page lists hundreds of appearances between January and April—and posting on Twitter, which he views as a form of crisis communication. On March 26, he became Twitter famous after he posted a 17-tweet thread detailing his concerns about the White House Coronavirus Task Force meeting at which President Trump announced he wanted "packed churches" on Easter. "I wasn't trying to have a confrontation. I have no interest in a political discussion," Inglesby says. "I was just trying to describe the risks of ending social distancing too soon. From the beginning of the coronavirus response I've tried to be straightforward with what I'm seeing and communicate the important decisions that are coming up, and the evidence for taking one or another course."
After his thread went viral, Inglesby's Twitter followers skyrocketed. The center's COVID-19 newsletter, which initially was sent to 6,000 people on January 23, is currently delivered to 150,000 inboxes every weekday. For decades, CHS experts and others in the health security field have struggled to raise awareness, to convince policymakers and the public to prepare for the devastating consequences of a pandemic. Now that it's happened, everyone is finally listening.
Eric Toner is frustrated that it's too little, too late.
"We've been talking about this for decades, and no one was paying enough attention. Some people said we were fear-mongering. Some said this was science fiction; it couldn't happen. Others saw it as such a low probability threat that it wasn't worth investing in," says Toner, an internist and emergency physician who practiced medicine for 23 years before becoming a senior scholar at CHS.
Of all the CHS experts, Toner is perhaps experiencing the strongest sense of déjà vu. He was the mastermind behind Event 201 and spent countless hours imagining the headlines he's now reading in real life. The overwhelmed ICUs, the personal protective equipment shortages, the lack of a vaccine, the limited ventilators. "So much of what we're seeing was predictable," says Toner, a hospital preparedness expert who has served as the principal investigator on several U.S. government–funded projects to assess and advance health care preparedness.
As the pandemic spread, Toner drew on his experience to make practical recommendations to lessen its impact. In early March he co-authored an article in JAMA outlining the priorities for the U.S. response to COVID-19, including reviewing preparedness plans, rapidly expanding diagnostic testing, and implementing social distancing to contain the spread. In mid-March he wrote a "wake-up call" article in Annals of Internal Medicine imploring hospitals to prepare for a surge. "Even into mid-March we were hearing that hospital emergency managers were panicking, but they weren't getting buy-in from their senior leadership, who were saying President Trump says this isn't a big deal," Toner says. "We were trying to amplify the message to hospital leaders. 'No kidding, you need to really start getting ready. And here's a list of many of the things you need to do.'" In April, following reports that the national stockpile of PPE was nearly empty, he published a CHS report estimating the supplies necessary to protect health care workers during a 100-day COVID-19 wave. His calculations, based on "middle of the road" rates of death and illness, showed that 3.4 billion pairs of gloves, 321 million isolation gowns, 179 million medical-grade masks, and 57 million N95 respirators would be required. The data, he hoped, would demonstrate the magnitude of the need and motivate decisive action before it was too late.
Data is at the heart of what CHS does—collecting it, analyzing it, and using it to create models and predictions that aid disaster prevention and planning. CHS senior scholar Jennifer Nuzzo, SPH '14 (DrPH), was one of the creators of the Global Health Security Index, a tool that uses open source data to score countries' capacities to prevent and respond to a health disaster. According to the index, which was released in 2019, the average score is 40.2 out of a possible 100, which means no country is amply prepared for epidemics or pandemics, she says. The U.S. ranked first in the world with a score of 83.5. Based on that rating, one wouldn't expect the U.S. to be as challenged as it is now, Nuzzo says. "I think more of our problems relate to leadership."
Not surprisingly, the index reveals most developing countries have strikingly less capacity to respond to a health disaster. "In the developing world there are weak health systems which, in the context of a pandemic like this, is particularly worrisome," she says. "But also, I'm deeply worried about the feasibility of using social distancing as a main tool for coping with the pandemic in countries when people are making their living in the streets. How can you tell people to stay home for two weeks if they can't eat?"
There is, however, evidence that countries that have experienced pandemics before may be in a better position to respond. Uganda snapped into action early, she says, and has robust contact tracing and a community health force. "They may actually be OK," she says. "There are many aspects where they have better capacity because they have regular experience with bottom-up approaches."
Another innovative tool in the CHS arsenal is the Collective Intelligence for Disease Prediction Platform, which was spearheaded by Tara Kirk Sell, SPH '16 (PhD), a senior scholar at CHS (and former Olympic swimmer). As Sell explained when she testified in front of the U.S. House of Representatives Committee on Science, Space, and Technology on March 5, the platform uses collective intelligence to inform infectious disease preparedness and interventions. After CHS launched the Disease Prediction Platform in January 2019, they asked volunteer forecasters from a range of fields all over the world—public health, medicine, academia, and others—to regularly respond to questions about ongoing disease outbreaks, including Ebola in Democratic Republic of Congo and measles in the United States. On most occasions, Sell says, the group of roughly 500 forecasters accurately predicted the infectious disease outcome—on average about three weeks before the outcome actually occurred. "Together the crowd is more accurate than any individual," Sell says.
Early in the COVID-19 outbreak, forecasters on the platform showed high confidence that there would be rapid and explosive spread. "Even though there were only a couple thousand positive tests in the United States at that point, forecasters were very certain there'd be many many more," Sell says. "That certainty was a clear signal that there was a lot of disease out there." On the other hand, when Sell asked forecasters to estimate both numbers of cases of COVID-19 and its fatality rate, the answers fell into a wide range. "That tells us there wasn't enough information out there for people to have certainty," she says. In her testimony to Congress, Sell stressed that in order for tools like crowd-forecasting to be beneficial, there has to be funding and support to gather accurate disease surveillance data. Without it, she says, forecasters don't have information to make accurate or useful predictions. "It's garbage in, garbage out," she says.
How to think about your activities and COVID risks this summer: consider ventilation, level of close contact, number of people, and amount of time. Make sure to think about you and your family's underlying risk factors too. https://t.co/iMPCCcAR2L
— Tara Kirk Sell (@skirkell) May 28, 2020
Sell also studies misinformation during disease outbreaks, everything from the promotion of fake cures, to rumors about the origin of the disease, to disinformation created to mislead—all of which can inhibit public health measures intended to promote safety. "It's clear that there are some serious concerns about misinformation and disinformation around COVID," she says.
One conspiracy theory hit close to home. On January 24, an article on the far right conspiracy theory site Infowars.com (which receives approximately 10 million visits per month) alleged Event 201 was proof that CHS had "predicted" COVID-19. CHS refuted the claim in a public statement, taking special care to clarify that the death count from Event 201—65 million—was not a predicted outcome for COVID-19. A related conspiracy theory alleged Event 201 was a dry run for a virus the Bill & Melinda Gates Foundation had engineered in order to profit from vaccine development. That rumor got enough traction that USA Today ran a fact-check, concluding the rumors were false. Instagram removed the post, a move that echoed CHS's recommendation, in the wake of Event 201, for governments and traditional and social media companies to develop nimble and effective approaches to containing such misinformation.
"You can think of disinformation and misinformation as a virus that needs a susceptible host to take hold and cause harm," says Monica Schoch-Spana, A&S '93 (MA), '99 (PhD), a CHS senior scholar and medical anthropologist who studies how communities respond to and recover from extreme events. "Disinformation takes root in contexts of distrust and social fragmentation. That's what we have now in the United States, which means we have a lot of susceptible hosts."
The fact that COVID-19 is a novel virus—something no one has seen before—increases people's anxiety and fear, which can lead to stigmatization and xenophobia. "People project the disease onto outsiders, especially in the case of a new virus," Schoch-Spana says. In 2009 with H1N1, the first cases emerged in Mexico, and people in America were blaming Mexicans and Mexican Americans for spreading the disease. "People called it the Mexican Flu, the Fajita Flu," she says. "It's analogous to what happened with COVID-19 in China. Today you get people calling it the Chinese Flu, the Wuhan Flu, and the Kung Flu."
The stark difference between H1N1 and COVID-19, she says, is top leaders' responses to the stigmatization. In 2009, President Obama sought to mitigate it by distributing accurate information and meeting with Mexican American leaders in a public town hall. "There wasn't any intention of fragmenting society, or taking advantage of existing fragmentation, as there is today with top officials continuing to call it the Chinese virus," she says.
That fragmentation shows in the range of responses to COVID-19, Schoch-Spana says. Some conservative commentators initially claimed the virus was being overblown to make the president look bad. Some liberal leaders and commentators believe Republican districts are getting more resources from the federal government than Democratic ones are. Some leaders put more stock in science than others. Schoch-Spana, who has studied epidemic response for decades, says she is stunned by the disunified response to COVID-19. "This is the most politicized response to a disease that I've ever seen in the United States," she says.
In early May, as groups of protesters throughout the country demanded an end to social distancing measures, claiming the public health measures were destroying their economic well-being, Schoch-Spana noted they were "drawing on a strong American ethos of rugged individualism, personal choice, and freedom from government intervention." But at the same time, she says, "these cultural constructs or values can be manipulated and employed by different social factions and serve overt political ends. I believe that the binary choice between economic well-being and public health is a false one, and we must be skeptical about the vested interests served by pitting the two objectives against one another."
And yet, she says, there is more good behavior in the wake of catastrophes than bad behavior. Community groups are helping provide groceries, supplies, and moral support, and you have others sewing and donating masks. "It's good stuff. It restores my faith in community," she says.
As the scientists and researchers at CHS know—and as the rest of the world is learning—a pandemic has stages, chapters of a story that unfold in a predictable order, if not a predictable timeline. At the end of March, as much of the nation adjusted to social distancing, CHS scholars Caitlin Rivers and Crystal Watson were thinking ahead to the next stage as they drafted a blueprint advising a careful and cautious staged reopening of states and regions even as they anticipated people's desire to return to normal as quickly as possible. "We know the physical distancing measures are having a severe economic impact, along with the virus itself," Watson says. "At the same time we need to realize that if we let up on them too soon, it will contribute to many more deaths, and we will have wasted our time and sacrifice."
The blueprint, which was a collaboration with the American Enterprise Institute, advised a state or region to begin reopening only after it met a series of benchmarks: a sustained reduction in cases for 14 days, scaled-up hospital and testing capacity, and an ability to monitor confirmed cases and their contacts. To build capacity for contact tracing, Watson and her colleagues proposed a radical idea: hire 100,000 "lay" contact tracers to perform identification and monitoring. The skills can easily be taught on the job, a high school–level education suffices, and no previous public health education is necessary, she says.
In a CHS report published in mid-April that offered specific guidance to governors about reopening, Watson and Rivers and their CHS colleagues urged states to actively monitor and manage COVID-19 cases to keep the reproduction rate under control—otherwise, they warned, the epidemic would resume and large-scale physical distancing measures would have to be reinstated. "Getting things open again will increase the risks of individuals contracting COVID-19, and there is no way to completely guard against that," the report said.
As far as the return to some semblance of normal life, Watson says that will only happen once we've got the therapeutics or vaccines. But, she warns, the return to normality should not be seen as the final stage of COVID-19. The final stage is preparation for the next pandemic: building our ability to create new vaccines for novel viruses within months, not years, and integrating new technologies into many areas of epidemic response, including surveillance, diagnosis, and treatment. And, says her colleague Rivers, it should mean the formation of a National Infectious Disease Forecasting Center, modeled on the National Weather Service, with a dedicated team of outbreak scientists. "We look to the weather service to determine what we should wear, and if we should bring an umbrella," says Rivers, an epidemiologist. "You can imagine a future where the National Infectious Disease Forecasting Center would send a text to your phone notifying you that there's an uptick in influenza in your area, and you might want to stay home or take hand sanitizer."
As the pandemic unfolded, like many of her CHS colleagues, Rivers felt a combination of complicated emotions. "Through our tabletop exercises, we foresaw the economic consequences and the challenging decisions we're facing. We anticipated the broad strokes of this ... but it hasn't blunted the impact of the details," she says. "On the one hand everything has surprised me. On the other hand, nothing has."
Reflecting on Event 201 from the vantage point of nine months—and what feels like an epoch—away, Toner says he wished he'd thought bigger. Rather than being guilty of doomsdaying or catastrophizing, he believes he was guilty of a "constrained imagination" in scripting the simulation. "We always used the 1918 flu pandemic as the worst-case scenario," he says. "Now we're seeing 1918 wasn't the worst case. COVID is the new worst case."
And yet, Inglesby says, it could have been worse. Even as he's painfully aware of the shortcomings, the vulnerabilities, and the lack of preparedness, he recognizes that without health security experts working tirelessly throughout the past two decades to raise awareness, propose innovative solutions, and urge the world to prepare, the impact of COVID-19 would be far more catastrophic.
"This is a terrible position for the country, but there are lots of things in place that if this had happened in 2000 we would be in a much worse position," he says. "The fact that the new vaccine is estimated in 12 to 18 months would have sounded like science fiction 10 years ago. The fact that we're already putting products and therapies into trials ... is impressive. It's a far step forward. Is it enough? Absolutely not."
Before COVID-19 Inglesby and his colleagues preached preparation and prevention. Now their mantra is "respect the virus." In early May, as states began reopening, Inglesby appeared on NBC's Meet the Press to warn that easing social distancing would cause waves of virus to emerge throughout the summer. "This virus is highly transmissible," he said. "Nothing has changed in the underlying dynamics of this virus. If we stopped social distancing altogether tomorrow, we would recreate the conditions that existed in the country in February and March." He took to Twitter to post an epic 18-tweet thread cautioning against the belief that the nation would soon be "in the clear" from COVID-19. "On March 1, the US had 100 recognized cases," he tweeted. "2 months later we have 1.1M recognized cases. We will need to respect the high capacity this virus has to do harm in the US until we have a vaccine." Come fall, he says, the world will have to reckon with two major concurrent public health challenges: COVID-19 and seasonal influenza.
For decades, Inglesby and his epidemic expert colleagues tried to warn the world about a pandemic like COVID-19—but most of us just couldn't imagine it. That was the power of Event 201. In experiencing a fake pandemic, participants were able to imagine a real one, and act to mitigate it.
CHS doesn't have any plans to create a new tabletop exercise. They're too busy with helping navigate us out of a real public health disaster. Instead, their challenge, once the nation and world are truly in the clear, will be to keep pandemic prevention and planning at the forefront. They are all too familiar with the cycle of panic and neglect that has characterized the response to outbreaks: During and immediately after an outbreak, it's top priority for policy- and budgetmakers. But once the panic subsides, the neglect sets in.
We can't afford to continue that cycle, says Inglesby. "It's obvious what the stakes are."
Posted in Health, Politics+Society