All of the following happened during a three-week stretch in August:
A nurse at Texas Children's Hospital in Houston posted a comment on an anti-vaccine Facebook page about the city's first measles case in five years. She said the young boy, whom she described as "super sick," was the first case of measles she and others at the hospital had ever seen. But she said that despite the child's "terrible" condition, she still had no regrets about opposing the use of vaccines. The nurse was subsequently fired. According to the hospital, it was because she had posted health information about a patient on social media.
The upper house of Italy's parliament voted to suspend a requirement that children receive 10 vaccines before they enter preschool. The populist coalition now controlling the government supports the position that the decision to vaccinate should be left to a child's parents.
A study published in the American Journal of Public Health found that the propaganda efforts of Russian internet trolls and bots have included tweets weighing in on the subject of vaccine safety. While the bots focused on attracting clicks through provocative anti-vaccine comments, the approach of the trolls was more nuanced. According to the study, they disseminated both pro and con messages, with the goal of sowing discord and creating a false sense of equivalency.
The World Health Organization reported that the number of measles cases in Europe reached a record high through the first six months of 2018. More than 41,000 children and adults contracted the disease from January through June, almost double the total for the region during all of 2017. Thirty-seven people died from measles during the same period.
These are confounding times when it comes to vaccines. Critics of their required use have made inroads with the public, and yet the medical community hasn't wavered in its belief that they are safe and effective. In fact, a 2014 Pew Research Center survey found that 86 percent of medical scientists believe vaccines should be mandatory.
Vaccines also are clearly effective. Take, for instance, their impact on the spread of measles. In the decade before 1963, when a vaccine first became available, an estimated 3 to 4 million Americans became infected with the disease every year, according to the Centers for Disease Control and Prevention. An estimated 400 to 500 people died each year—most of them children—and another 48,000 were hospitalized. By 2000, the number of new measles cases per year had plummeted to fewer than 100.
Overall, vaccines have eradicated or brought under control seven major human diseases—smallpox, diphtheria, tetanus, yellow fever, whooping cough, polio, and measles. It's been estimated that the elimination of smallpox has saved 40 million lives. Deaths from polio worldwide have dropped by 99 percent since 1988—only 22 were reported in 2017—and more than 16 million people have been saved from paralysis, according to the WHO.

Despite those impressive statistics, anti-vaccine activists have been successful in raising doubts about vaccination safety, primarily by promoting a debunked myth of a link between measles vaccine and autism.
The recent spike in measles cases in Europe and several outbreaks of the disease in the U.S.—including one in early 2015 in which 147 people contracted measles traced to exposure at two Disney theme parks in California—is likely a reflection of that vaccine skepticism. A 2016 survey, called the Vaccine Confidence Project, found that 41 percent of the French population disagreed with the statement, "Overall, I think vaccines are safe." The percentages were also relatively high in Greece and Ukraine (one out of four people) and Italy (one out of five).
About 14 percent of Americans surveyed had doubts about vaccine safety, slightly above the global average of 12 percent. The measles vaccination rate in the U.S. remains above 91 percent—the WHO goal is 95 percent—but public health officials here worry about an uptick in communities where clusters of parents are choosing not to have their children vaccinated.
Daniel Salmon believes that the number of Americans adamantly opposed to vaccinations is actually quite small, maybe lower than 1 percent. But as director of the Institute for Vaccine Safety at the Johns Hopkins Bloomberg School of Public Health, he is painfully aware of how well the anti-vaccine movement has been able to aggressively use the internet and social media to raise uneasiness or suspicion among those known as the "vaccine-hesitant."
He points out that it's not unusual for young parents to be anxious about their babies getting inoculated. Maybe as many as one in three has serious concerns about it, Salmon suggests. "Think about the number of vaccines given to a child at one time, in their first few months," he says. "Parents want to protect their child. It's understandable why people have concerns. That doesn't make them anti-vaccine."
But that natural parental anxiety has been intensified by a darker fear, one that has its roots in a 1998 study published in The Lancet, the British medical journal. That research, led by Andrew Wakefield, then a gastroenterologist, suggested a connection between MMR vaccine (measles/ mumps/rubella) and the onset of autism. Ultimately, after an investigation called into serious question both the research and Wakefield's ethics—he never disclosed funding by lawyers hired by parents suing vaccine-producing companies—the study was retracted by The Lancet, and he lost his medical license. Wakefield, who has since moved to Austin, Texas, insists that he was the victim of a campaign by the medical establishment to discredit him and remains active as an anti-vaccine speaker. He and others in the anti-vaccine movement have been able to generate revenue through appearing at seminars and selling books and "wellness" supplements.
"The starting point was the Wakefield study," says Meghan Moran, an assistant professor in the Bloomberg School of Public Health and a researcher who focuses on the communication of health information to the public. "It was a study by a real scientist and published in a real medical journal. Folks who didn't like vaccines to begin with were able to point to a specific study. We later found out it was fabricated and withdrawn from the literature. But the fact that it was withdrawn can be twisted into the belief that the medical industry doesn't want the real knowledge to come out. Because of social media, that idea can be disseminated much more rapidly and more widely today."
One recent example of how scientists have begun to push back against the autism claim in more personal ways is the publication of a book titled Vaccines Did Not Cause Rachel's Autism. Written by Peter Hotez, director of the Texas Children's Hospital Center for Vaccine Development at Baylor College of Medicine, it presents his perspective both as a scientist and the father of an autistic child. "Yes, the anti-vaccine and anti-science people are aggressive and have had an impact," he says. "But their activities actually stimulated me to write this book."

The truth is, vaccine skeptics have been around as long as the treatment itself. Though he was not the first to do so, British physician Sir Edward Jenner was an early advocate of protecting people from smallpox by injecting them with cowpox—a related but milder virus. His first paper, describing a successful inoculation in 1796, was rejected by the Royal Society in London as too revolutionary. Even after a later paper documenting more vaccinations was published, Jenner was widely ridiculed, particularly by the clergy, who found the practice "unnatural" and "unchristian." A cartoon published in 1802 went so far as to show small cows sprouting from the mouths, noses, and ears of people who had been inoculated.

Image caption: The caption on this 1802 cartoon by James Gillray shows it was printed by "the Publications of ye Anti-Vaccine Society"
Image credit: Wikimedia Commons
Once smallpox vaccinations were adopted by the medical community, anti-vaccine organizations and journals sprang up in Europe and the U.S., particularly after communities began passing laws making smallpox vaccinations mandatory. Some still distrusted the science; others objected to what they saw as a loss of personal freedom when it became illegal to refuse vaccinations for children.
In time, vaccination opposition waned, only to surge again late in the 20th century—first in the 1970s when questions were raised about the safety of DTP vaccine (diphtheria/tetanus/ pertussis or whooping cough), then more recently, with Wakefield's discredited claim about autism.
The irony is that vaccines have likely come under more scrutiny because of their success. Smallpox has been gone from the U.S. and Europe for almost 70 years, and a shrinking number of people have personal memories of the polio epidemics of the 1940s and 1950s that killed or paralyzed as many as half a million people a year, most of them children. By 2000, measles was considered eliminated in the U.S. "Fear shifts from the diseases that are effectively controlled to the vaccines themselves," Salmon says. Another complication, he notes, is that the first signs of developmental problems, such as autism, occur around the same time that an infant is vaccinated. So, people have found it easier to believe a connection between the two. "It's a normal, understandable fallacy, but it presents a problem for vaccines. We also tend to fear things we have no control over. With vaccines, people feel they have no control."
Andrew Read, director of the Center for Infectious Disease Dynamics at Penn State University, also teaches vaccine safety. He raises another issue—the difference in how scientists and the general public perceive risk. Researchers know there's always a risk of side effects from vaccines, albeit very small. Occasionally, a child receiving the measles vaccine could experience seizures or a temporary low platelet count, and in extremely rare cases, deafness or a coma, according to the CDC. But the anti-vaccine movement has raised expectations that no risk should be acceptable. And that notion, while quite unrealistic, has become part of the public discourse. "To me, it's a miracle that a small injection of a clear liquid can protect you for life from these debilitating diseases," Read says. "The risks of vaccines are actually pretty small compared to a lot of things you do in life. But people hear stories, and horror stories are horror stories."
That's in line with Moran's experience. "Understanding risk can be tough for a person who may have no experience with a disease like measles," she says. "They haven't known anyone who has had it. That could be going up against some anecdote about a kid who has had one of the very rare side effects. That story is a lot more vivid."
Moran knows what medical and public health professionals are up against when it comes to countering vaccine deniers. A few years ago, she led a team that analyzed nearly 500 anti-vaccination websites. It was a sobering undertaking. About two-thirds insisted that vaccines cause autism. Many of the sites also took findings from peer-reviewed research and misinterpreted or distorted them. One other feature of at least a third of the sites is that they relied heavily on personal anecdotes, rather than emphasizing scientific research.

While the toll of anti-vaccine sentiment related to measles has been considerably less in the U.S. than in Europe, the incidence of the disease has been creeping up since dropping to only 86 cases nationwide in 2016. Through mid-August, 124 cases had been reported in 2018, including nine different "outbreaks"—that's three or more linked cases.
One concerning trend is a rise in the number of nonmedical exemptions. These have been granted to parents who for religious or philosophical reasons request that their children not be vaccinated. Currently, 18 U.S. states permit philosophical exemptions and, according to a study published in PLOS Medicine last June, the number in 12 of those states has increased since 2009. The states with rising philosophical exemptions are Arkansas, Arizona, Idaho, Maine, Minnesota, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Texas, and Utah.
Also see
The study also identified what were described as "hot spots"—communities with larger than ordinary numbers of these exemptions and, therefore, more susceptible to outbreaks. These included rural communities in Wisconsin, Idaho, and Utah, and also metropolitan areas, such as Seattle, Portland, Houston, Austin, Fort Worth, Phoenix, Salt Lake City, Detroit, Kansas City, and Pittsburgh.
It's still a small number of children who aren't vaccinated for philosophical reasons—fewer than 50,000 kindergartners nationwide—but it's growing. In Texas, for instance, the percentage of children opting out of vaccinations for nonmedical reasons doubled from the 2011–12 school year to last year.
The problem comes when there are clusters of unvaccinated children in a community. That minimizes the effect of what's known as "herd immunity"—when roughly 90 percent of a population has been inoculated, greatly reducing the chance of a contagious disease spreading. Without that, outbreaks are more likely, such as one in which 383 Amish residents of central Ohio were infected with measles in 2014, and another in Minneapolis in 2017 when 79 Somali-American children contracted the disease.
Often overlooked is how much strain disease outbreaks can place on local public health departments. An analysis published in JAMA Pediatrics last summer found that during a 2013 measles outbreak of 58 cases in an Orthodox Jewish community in Brooklyn, 87 members of the New York City Department of Health and Mental Hygiene spent more than 10,000 total hours tracking and trying to control the spread of the disease. The cost to the city? Just under $400,000.
The outbreak among Somali-Americans in Minnesota was particularly frustrating for local clinicians and public health officials. At one point, that community had had one of the higher vaccination rates in the state. But by 2014, only 42 percent of its children were being inoculated against measles. The big reason was fear of autism. Some members of the close-knit group had read about the rumored link between vaccination and autism on the internet, and their fears were fanned by anti-vaccine activists in the Minneapolis area. Those activists even invited Andrew Wakefield himself to meet with Somali-American families, which he did several times in 2010 and 2011. The clear message was that if parents didn't want to vaccinate their kids, they didn't need to. It was only after imams from local mosques began endorsing vaccines that fear of inoculations started to ease.
As director of the University of Minnesota's Center for Infectious Disease Research and Policy, Michael Osterholm witnessed firsthand how mistrust helped fuel the outbreak. "One thing we need to take seriously is that we always thought that more education was all it would take for people to come to the right answer," he says. "We now realize that's simply not the case."

Those who oppose mandatory vaccinations often say they aren't actually anti-vaccine but rather pro-choice—that it should be a decision left up to the parents. It's a position that appeals to a broad spectrum of skeptics, according to Paul Offit, director of the Vaccine Education Center at Children's Hospital of Philadelphia: "On the right, it's more of a libertarian argument: 'I don't think I should be made to have a biological fluid injected into myself or my child. Let me do my own research and I will make the best decision for my family. Get the government off my back.' On the left, it's 'I want all things natural. Injecting a biological thing into my child's arm is not a natural thing to do.' Two different arguments, both ill-founded."
The challenge is that the persistent and strategic use of social media by the anti-vaccine movement has enabled it to have an outsize influence. Michael Kinch, director of Washington University's Center for Research Innovation in Business, remembers the reaction to his recent book, Between Hope and Fear: A History of Vaccines and Human Immunity. "Within the first few hours the book was out, the anti-vaxxers went on Amazon and smeared it," he says. "This group is very organized. Anyone who underestimates them does so at their own risk. When they do things like this, you just have to assume that they mean well. They're convinced that vaccines cause harm."
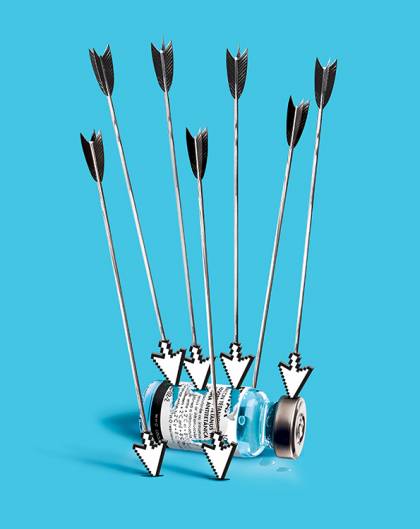
Image credit: Doug Chayka
Beyond that, it's been suggested that the ability of activists to cherry-pick negative results from vaccine studies may be having a chilling effect on research. In an op-ed article in The New York Times in August, science and health writer Melinda Wenner Moyer wrote: "Scientists are so terrified of the public's vaccine hesitancy that they are censoring themselves, playing down undesirable findings and perhaps even avoiding undertaking studies that could show unwanted effects." Osterholm acknowledges that he has been "shot many times from both the back and the front," including, he says, by colleagues. "Some supporters of vaccines have actually done us a disfavor in some cases," he says. "They have made it seem that any criticism of a vaccine is more detrimental than it is helpful. And I absolutely disagree with that. The most important thing is that we tell the truth."
Kinch agrees that it's important to acknowledge risk when it exists. "To suppress negative research is scientific malpractice in my opinion," he says. "The fact is that there's never a perfect solution to anything. Just because a vaccine isn't perfect doesn't mean you don't take it. What makes science unique is that as we go along, we refine ideas. The beauty of science is that you're continually improving."

While the depth of vaccine angst is hard to measure, it apparently has risen to the point where it's now considered a topic polarizing enough to be exploited by Russian internet trolls and bots. That was the surprising conclusion of the aforementioned study, which found that those disinformation social media tools disproportionately mentioned vaccines.
"The agenda of Russian trolls is to sow conflict and mistrust among the population," says Mark Dredze, an associate professor of computer science at the Whiting School of Engineering and one of the study's researchers. "So the fact that they chose a health topic was a wake-up call to us. This isn't just a foreign power trying to interfere with an election and being disruptive to politics. It's a broader effort to polarize society around a host of topics. And vaccinations are now one of them.
"It should be scary to us that medicine and health could become polarized," he adds. "Vaccines have not really been a partisan issue. The fact that outside powers are trying to push us in that direction is a huge concern. Once this door has been opened and this has been identified as a topic that can be divisive, I fully expect people to do it again."
Prior to his election, President Donald Trump tweeted vaccine messages dozens of times, including one in 2014 when he said: "Healthy young child goes to doctor, gets pumped with massive shots of many vaccines, doesn't feel good and changes—AUTISM." He met with Andrew Wakefield and later invited him to one of his inaugural balls. A survey in December 2016 by YouGov, a global public opinion and data firm, found that one out of three Trump supporters believed vaccines could cause autism. Just before he was inaugurated, Trump also told Robert Kennedy Jr., another high-profile vaccine skeptic, that he wanted him to head up a commission to review vaccine safety. To date, no such commission has been created.
In Europe, however, politicians in a number of countries, including Italy and France, have made a point of weaving anti-vaccine stances into populist agendas. In France, right-wing presidential candidate Marine Le Pen campaigned against mandatory vaccinations. The Five Star Movement, Italy's most popular party, has opposed policies increasing the number of required vaccines, and Matteo Salvini, the country's deputy prime minister and minister of the interior and one of its most powerful politicians, has declared vaccinations "useless and, in many cases, dangerous."
Perhaps not surprisingly, measles cases have shot up in Europe in the past few years, from 5,273 in all of 2016 to almost eight times that number during just the first six months of 2018. More than half of those cases were in Ukraine, but in six other countries—France, Italy, Greece, Russia, Georgia, and Serbia—more than 1,000 people were infected with measles in the first half of this year.
"Any time science is politicized, it can be harder to do our jobs because it touches on that trust issue," Moran says. "We need to work harder on communicating that we are looking out for everybody."
Salmon agrees. "It's a real challenge for public health. Trust in government is at an all-time low. And the public health agencies that strongly promote vaccines are government agencies. One of the outstanding questions is how do we maintain and improve trust in public health agencies."
So, it has become that much more important to find the most effective ways to ease the anxiety of parents. Salmon says it starts with health professionals taking those concerns seriously, then responding appropriately. "We need to identify those concerns and address them, not in isolation but in the context of a larger message that emphasizes the risk of disease, and the benefits of vaccines in addressing the specific concerns you have. That's what the evidence shows is most likely to work. Simply hitting back at myths can backfire. For example, if a person is concerned that a flu vaccine can cause the flu, we don't have the doctor say, 'I understand why you worry about the flu vaccine giving you the flu' because even if they go on to debunk that myth, by mentioning it you reinforce it.
"So, instead the doctor might say, 'I understand why you want to prevent the flu. Let me explain to you that the vaccine can't cause the flu. The best way to prevent the flu is the vaccine.' You want to show empathy, but do so carefully."
Both Salmon and Meghan Moran think timing also is critical. Ideally, a doctor should discuss vaccinations when a woman is pregnant with her first child, which Salmon describes as a "teachable moment." An expectant mother usually hasn't given much thought to vaccines at that point, and probably hasn't already formed negative opinions. "People are more likely to latch on to something if it fits with what they already believe," Moran says. "If they already are a little iffy about vaccines, they might be more likely to blow something negative out of proportion."
They also say it's increasingly important for medical professionals to address any fears empathetically, rather than dismissing them or trying to simply counter them with scientific data. "One or two bad experiences can be enough to break somebody's trust, and it can fuzz out into mistrust of the whole system," Moran says. "Someone whose doctor doesn't take their concerns seriously may then have an experience with an alternative health care provider who does take them seriously. And then there's now this whole other system they're placing their trust in that may or may not be evidence-based."
While she believes it's important to be very clear about the facts of vaccination, Moran thinks coupling them with an anecdote can make them more memorable. "It's one thing to read a bulleted list of what can happen if you get measles, but it's another thing for someone to hear a parent talk about how their baby was too young to get vaccinated and came into contact on the playground with someone with measles. And their baby contracted measles and they had to rush him to the ER and they stuck tubes down his throat. Having someone tell that story in vivid detail has much more impact. If the listener is a parent, they know what it's like to see their child in pain."
Moran also feels that, like it or not, health professionals need to realize there sometimes may be better people to deliver a vaccine safety message. The impact of the imams in Minnesota is a telling example. "You need to find people with whom they already have a trust relationship," she says. "They could be in churches or schools, even beauty salons. You need people who can help you get around the distrust of the medical community.
"It's our job to meet people where they are. If you're doing public health and you're not getting your message across, it's not your audience's fault."
Posted in Health, Politics+Society











