Johns Hopkins biomedical engineer Sri Sarma is developing new technologies to pinpoint the exact origin of seizures in the brain—life-changing work for the roughly 21 million epilepsy patients worldwide whose seizures aren't relieved by medications.
Removing the specific brain region where seizures originate is the last resort when medication fails. But current clinical tools make precisely locating the epileptogenic zone (EZ) extremely difficult, rendering surgery effective in only about half the cases. With funding from the National Institutes of Health, Sarma and her team help surgeons determine if and where they should operate, improving the success rate of epilepsy surgeries.
Video credit: Roy Henry / Johns Hopkins University
"Today, accurately diagnosing epilepsy and then finding an effective treatment can take years to a lifetime," said Sarma, director of the Neuromedical Control Systems Lab who also serves as vice dean for graduate education at the Whiting School of Engineering. "To fill this gap, we focus on developing computational tools that allow for earlier, precise diagnosis and assist doctors in figuring out the best treatment for each patient."
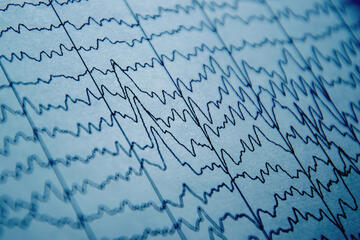
Epilepsy is a disorder characterized by sudden recurrent episodes of seizures, or abnormal electrical activity in the brain. Sarma and her team use machine learning and non-invasive electroencephalography (EEG)—a technique that involves attaching electrodes to a patient's scalp—to capture electrical brain activity related to epileptic seizures. The cornerstone of their work is integrating these findings into diagnostic and surgical planning tools that can be used in the clinic.
Among the innovations developed by Sarma's lab is the software EZTrack, which creates a heat map of the brain to help doctors identify a patient's EZ in seconds with high precision. In addition to EZTrack, the team is currently building out EpiScalp, a software tool that provides an accurate epilepsy diagnosis from a single initial EEG recording, significantly cutting down on misdiagnoses that often delay treatment.
"Our work is unique in that this is a new way of mapping epilepsy activity and networks that is personalized to each individual patient's brain," Sarma said. "More important, though, is the tremendous potential to guide successful epilepsy surgeries so more patients can live seizure-free."
In 2022, the NIH selected Sarma to be the technical director of NeuroTech Harbor, a Baltimore-based technology accelerator working to fast-track the next wave of breakthrough technologies for neurological disorders. Led jointly by Johns Hopkins and Howard University, NeuroTech Harbor is helping aspiring entrepreneurs launch 45 neurotech projects in just five years.
Outside of her lab, Sarma has emerged as a mentor for tomorrow's neurotech leaders, spearheading educational and outreach activities for young women in science and engineering. She has led the organization of the Rising Stars in Engineering in Health Workshop, an annual event to support women pursuing academic careers in science and engineering; as well as several mentoring projects with support from Loreal's Changing the Face of STEM grants.
Sarma, who has been with Johns Hopkins since 2009, said that the university is a powerhouse in translating the latest neuroscience research into treatments and cures. It's also where so many future innovators find their start.
"Thanks to research funding, we're setting a new standard in early diagnostics and personalized care for neurological conditions," Sarma said. "But funding doesn't just enable us to make discoveries—it supports the mentoring and growth of the next generation of leaders. We can't afford to underestimate the importance of building up America's STEM workforce."
Posted in Health, Science+Technology
Tagged epilepsy, nih funding