- Name
- Jill Rosen
- jrosen@jhu.edu
- Office phone
- 443-997-9906
- Cell phone
- 443-547-8805
A new artificial intelligence-based approach can predict if and when a patient could die of cardiac arrest. The technology, built on raw images of patient's diseased hearts and patient backgrounds, significantly improves on doctor's predictions and stands to revolutionize clinical decision making and increase survival from sudden and lethal cardiac arrhythmias, one of medicine's deadliest and most puzzling conditions.
The work, led by Johns Hopkins University researchers, is detailed today in Nature Cardiovascular Research.
"Sudden cardiac death caused by arrhythmia accounts for as many as 20% of all deaths worldwide and we know little about why it's happening or how to tell who's at risk," said senior author Natalia Trayanova, a professor of biomedical engineering and medicine. "There are patients who may be at low risk of sudden cardiac death getting defibrillators that they might not need and then there are high-risk patients that aren't getting the treatment they need and could die in the prime of their life. What our algorithm can do is determine who is at risk for cardiac death and when it will occur, allowing doctors to decide exactly what needs to be done."
The team is the first to use neural networks to build a personalized survival assessment for each patient with heart disease. These risk measures provide with high accuracy the chance for a sudden cardiac death over 10 years, and when it's most likely to happen.
The deep learning technology is called Survival Study of Cardiac Arrhythmia Risk, or SSCAR. The name alludes to cardiac scarring caused by heart disease that often results in lethal arrhythmias, and the key to the algorithm's predictions.
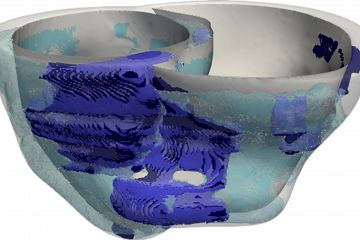
The team used contrast-enhanced cardiac images that visualize scar distribution from hundreds of real patients at Johns Hopkins Hospital with cardiac scarring to train an algorithm to detect patterns and relationships not visible to the naked eye. Current clinical cardiac image analysis extracts only simple scar features like volume and mass, severely underutilizing what's demonstrated in this work to be critical data.
"The images carry critical information that doctors haven't been able to access," said first author Dan Popescu, a former Johns Hopkins doctoral student. "This scarring can be distributed in different ways and it says something about a patient's chance for survival. There is information hidden in it."
The team trained a second neural network to learn from 10 years of standard clinical patient data, 22 factors such as patients' age, weight, race, and prescription drug use.
The algorithms' predictions were not only significantly more accurate on every measure than doctors, they were validated in tests with an independent patient cohort from 60 health centers across the United States, with different cardiac histories and different imaging data, suggesting the platform could be adopted anywhere.
"This has the potential to significantly shape clinical decision-making regarding arrhythmia risk and represents an essential step towards bringing patient trajectory prognostication into the age of artificial intelligence," said Trayanova, co-director of the Alliance for Cardiovascular Diagnostic and Treatment Innovation. "It epitomizes the trend of merging artificial intelligence, engineering, and medicine as the future of healthcare."
The team is now working to build algorithms to detect other cardiac diseases. According to Trayanova, the deep-learning concept could be developed for other fields of medicine that rely on visual diagnosis.
Posted in Health, Science+Technology
Tagged natalia trayanova, cardiac health