The United States needs to do more to expand the international supply of COVID-19 vaccines to nations still struggling to begin robust vaccination efforts while the 188 million fully vaccinated U.S. citizens will soon have access to three booster products.

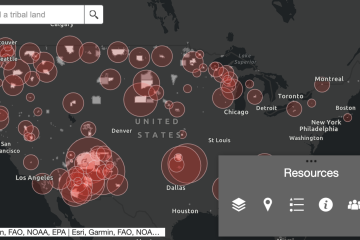
Image caption: Beth Blauer and William Moss
"We have a real luxury here in the United States that we're even talking about booster doses for our communities when much of the global community does not have access to vaccines," said William Moss, executive director of the International Vaccine Access Center at the university's Bloomberg School of Public Health, during the Coronavirus Resource Center's online briefing on Friday. "This remains a vexing problem that needs to be addressed."
Moss addressed the disparity in vaccine supplies during a briefing held at around the same time that a U.S. Food and Drug Administration committee voted to recommend a Johnson & Johnson booster shot. The same panel on Thursday unanimously supported a Moderna booster. Experts expect both products—like the Pfizer booster last month—to receive final approval from the FDA and the Centers for Disease Control and Prevention later this month.
But Moss said the federal government and public health officials need to better explain its goals for approving boosters while more than 40% of the U.S. population remains unvaccinated or not fully vaccinated. Too many people have not been vaccinated because of their misinformed belief that vaccines should provide perfect protection.
"Are we, with our vaccines, trying to prevent moderate and severe disease, hospitalizations, and deaths due to COVID, and really make this more of a mild disease that we can live with, like influenza?" Moss said. "I think that's where we are trying to go."
The number of COVID-19 cases and deaths in the United States have recently begun to decline. Over the past week, cases declined 13% and deaths dropped by 4%, according to an analysis of CRC data by Emily Pond, a research data analyst at the Center for Health Security in the Bloomberg School of Public Health. Still, cases and deaths are still above the pandemic's lowest point in mid-June when vaccination rates plummeted.
Without clear communications around the goal of minimizing COVID-19's impact, Moss said too many people end up expecting vaccines to provide "sterilizing immunity"—the unrealistic ability for a vaccine to prevent infection and stop transmission.
"We do not hold any other vaccine to such a high standard," Moss said. "This is why 'breakthrough' infections are expected and not necessarily a sign of vaccine failure."
The current vaccines reduce the likelihood of transmission, but they cannot prevent transmission completely. Boosters have been recommended primarily for people with various risks.
"But we don't yet have the evidence base to suggest that all adults should be getting booster doses," Moss added.
And what evidence does exist will also—like the vaccines themselves—not be perfect.
Beth Blauer, the CRC data lead and associate vice provost of public sector Innovation, joined Moss in the Friday briefing and raised alarms that vaccine data collection will only get less reliable as new categories of shots are added before standards are establishing for tracking the information.
Different states collect, classify, and publish vaccination data in several different ways, said Blauer, who has also written about her concern on the CRC's Pandemic Data Initiative.
"The real challenge around the collection of vaccination data is that there is a tremendous lack of standardization around how vaccination data is released to the public," Blauer said. "We're not able to do apples-to-apples comparisons within data sets."
A lack of standards, she added, "is going to create even more confusion around who is vaccinated and how many more miles we have to go in getting to the point where we feel we have a community that's safe or protected from a vaccination strategy that is effective."
Posted in Health, University News
Tagged coronavirus, william moss, covid-19 vaccine, coronavirus resource center, beth blauer