Almost as soon as reports began circulating earlier this year that a new coronavirus-linked respiratory illness was spreading from China, researchers at the Johns Hopkins Center for Humanitarian Health thought of the refugees living in Bangladesh. In the district of Cox's Bazar, nearly 1 million religious and ethnic minorities from Myanmar called the Rohingya live in refugee camps, with the majority—roughly 600,000—residing in the Kutupalong-Balukhali Expansion Site. At about 5 square miles, it is the world's largest refugee camp and one of the most densely populated places on the planet.
"A pandemic is particularly worrying, but really any type of disease transmission is concerning when it comes to refugees living in camps because they are often living in high density and with poor water and sanitation," says Paul Spiegel, director of the center and a professor of the practice in the Department of International Health in the Bloomberg School of Public Health. "We know from past experience that it's very common for epidemics to transmit easily in these settings."
Shaun Truelove, an assistant scientist in the departments of International Health and Epidemiology, had conducted previous research on diphtheria and found that the transmission of the bacterial infection was about 60% higher among the Rohingya than in other populations. He knew the introduction of a highly infectious virus to the region could be devastating.
"Knowing how this population has fared and been treated in the past, we were quite concerned that without prompt action by the international community, the pandemic could be a real disaster," Truelove says.

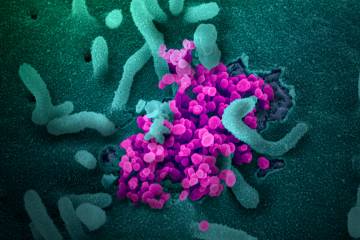
Image caption: Roughly 1 million Rohingya refugees live in Bangladesh, with the majority living within just 5 square miles in the Kutupalong Balukhali Expansion Site in the district of Cox's Bazar.
Image credit: UN Photo/KM Asad
To gain a better understanding of the scope of the threat, Truelove and the Infectious Disease Dynamics group led the development of a coronavirus transmission model based on the demographics of the expansion site, assumptions about the health care capacity in Cox's Bazar, and early data about the transmission potential of the virus, among other variables. Spiegel and scientists Orit Abrahim and Chiara Altare from the Center for Humanitarian Health helped interpret and operationalize the findings.
"The goal was to get an idea early on how bad it could be, in order to encourage organizations to rapidly engage and deploy resources that would increase health care infrastructure and isolation capabilities," Truelove says.
The model presented three transmission scenarios based on risk. In each scenario, a large-scale outbreak was almost guaranteed once the virus was introduced in the camp.
In the low-transmission scenario, the model suggested that at least 421,500 people could become infected. In the high-transmission scenario, that number reached 589,800—or nearly every person in the expansion site. The number of deaths was expected to be between 2,040 and 2,880. The model also suggested that without proper preparation and mobilization by the local health care system, the need for hospitalization would exceed capacity in 136 days in the low-transmission scenario and in just 55 days in the high-transmission scenario.
Spiegel shared the results with the United Nations high commissioner for refugees and the UNHCR's head of health. Their initial reactions, as well as Spiegel's, were to exercise caution in disseminating the model's findings.
"There has always been discrimination and stigma against refugees—for just being a refugee but also for spreading disease, which often is not the case," Spiegel says. "These situations can exacerbate the discrimination refugees face."
Officials in Bangladesh were already preparing for how the coronavirus might affect the Rohingya living in Cox's Bazar. The JHU team's model and three-tiered risk analysis helped officials think through the different transmission scenarios and develop strategies, Spiegel says.
"You plan according to what maybe could occur, but also according to your capacity. They set up isolation centers, they brought in some PCR machines for virus detection, and they increased the number of ICU beds available," Spiegel says. "If the worst-case scenario, which has not yet happened, does occur, they still would be in some significant trouble, I would say."
The first cases of coronavirus infection among the Rohingya were officially reported in mid-May, and empirical data collected by health care providers and officials in Bangladesh since then have indicated the spread of disease has been far lower than expected.

Image caption: Like other refugee groups, the Rohingya population has high numbers of young people and children, which could explain why the incidence of severe illness and death is much lower compared to non-displaced groups in China and the U.S.
Image credit: UN Photo/KM Asad
"Among a population of nearly a million people, the number of total coronavirus cases reported is around 145," Truelove says. "These are tiny, tiny numbers."
In some ways, this coincides with other findings from the team's model, which suggested a far lower fatality rate from the disease than was experienced in China early in the pandemic. Spiegel attributes the low fatality rate to the demographics of the Rohingya population, which is made up of far more young people and children than other population groups.
"Older people are those with concomitant diseases, and so it's maybe not surprising that the number of deaths that would occur in a setting with younger people is lower proportionally than in China, the U.S., and elsewhere," Spiegel says. "And the actual death rate among the Rohingya seems to bear that out."
He says it's also possible, though no evidence has suggested it to be the case, that some other form of coronavirus spread among the Rohingya, conferring a type of inoculation against the more severe forms of COVID-19.
Still, the Johns Hopkins Center for Humanitarian Health researchers and their colleagues in the Department of Epidemiology are rapidly developing plans to further investigate the conditions and factors that may be contributing to the low infection and fatality rates in Cox's Bazar. And their work has even more urgency, as similar scenarios are unfolding elsewhere in the world, including in densely populated parts of India and Kenya.
Ideally, Truelove says, the team would be able to analyze the results of serosurveys of the population and directly measure the number of people with COVID-19 antibodies, thus determining the scope of transmission. The resources to conduct such a survey aren't available yet, but the team is closely monitoring reports from Bangladesh.
For his part, Spiegel says he will continue to work with the UN and NGOs to examine the pandemic and look for any secondary effects of the pandemic among persons affected by humanitarian emergencies. Ongoing disease spread could prevent people from seeking preventive care or treatment in clinics, for example, or it could damage maternal and fetal health if expectant mothers refrain from having their babies delivered by skilled birth attendants. He and his colleagues are also paying close attention to the pandemic's social effects and thinking about how a vaccine, if available, would be perceived by refugees and other internally displaced people.
"There are a lot of indirect costs to human life we need to think about," he says. "It's been interesting to study—frustrating but also relieving. I'm obviously very happy it hasn't happened as we expected, but I would like to better understand more about why that is. And it's not that we can't do that kind of research, it's that there aren't enough resources to do it. But we'll get there."
Posted in Health
Tagged refugee crisis, center for humanitarian health, coronavirus, covid-19