This article originally appeared on the Johns Hopkins Medicine coronavirus website.
The swabs arrive at all hours, in double-bagged vials, sometimes hundreds at a time.
They come from the hospitals, clinics, and COVID-19 testing sites of the Johns Hopkins Health System. They come from patients at other hospitals in the region. They come in batches from residents and staff members of Maryland nursing homes, from people who are homeless, and from neighborhoods with COVID-19 clusters.
"You can imagine when we get bags of COVID samples, it gets really busy around here," says Heba Mostafa, assistant professor of pathology and director of the molecular virology laboratory at Johns Hopkins Hospital.
The Johns Hopkins microbiologists and staff members working in the windowless warren of the Johns Hopkins medical microbiology laboratory are ready. They sort the samples, prepare and test the genetic material, and deliver COVID-19 results—within an hour when necessary, and always in less than a day.
A team of about 90 people, including about 15 molecular microbiologists, works around the clock in the microbiology lab to process as many as 1,500 tests each day—a number that could double as the lab continues to add processing platforms, says Mostafa.
"Our turnaround time now for all testing is well below 24 hours," says Karen Carroll, professor of pathology and director of the Division of Medical Microbiology at Johns Hopkins. "We're trying to get to 12 hours, which will require a middle of the night run. The overnight shift is currently only doing the one-hour testing. "
Other testing sites nationwide often take between two and five days.

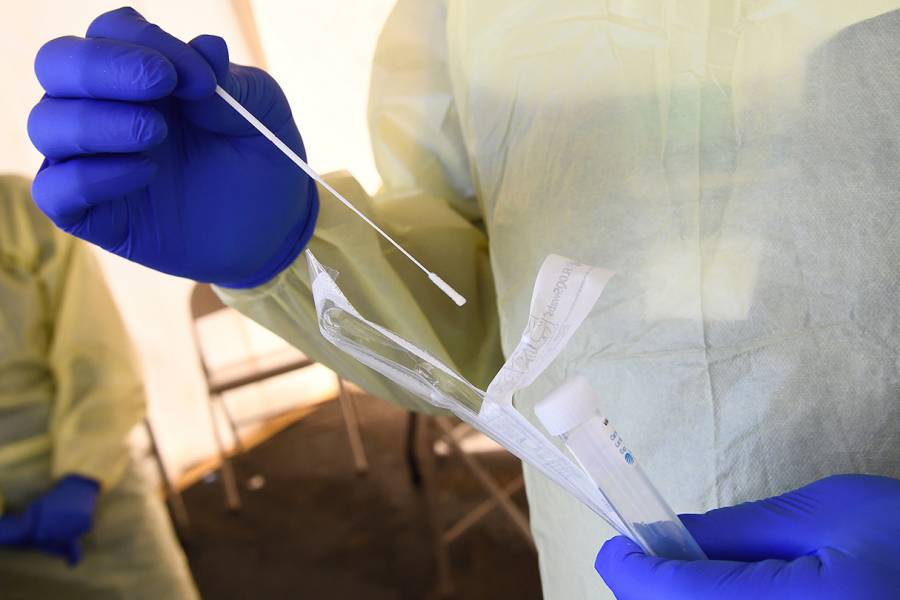
Image caption: Johns Hopkins doctors provide drive-through testing for COVID-19.
Image credit: Will Kirk / Johns Hopkins University
Johns Hopkins has been conducting its own COVID-19 tests since March 11, when clinical microbiologists Carroll and Mostafa developed an in-house screening.
That early test, which returned results within 48 hours, provided desperately needed information at a time when tests were in short supply. The results informed care and helped slow the spread of the coronavirus that causes COVID-19 through quarantine of people who tested positive.
"We have tested over 60,000 samples now," Carroll said in late June. "Dr. Mostafa and the molecular team have performed a record number of tests in a very short time."
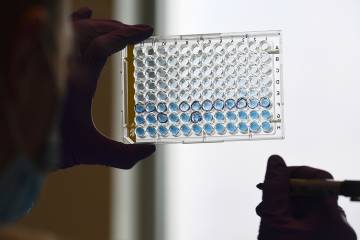
The lab currently uses nine testing systems to obtain results, each with its own strengths. Some produce answers more quickly, while others process more tests simultaneously.
One advantage to having so many kinds of tests, says Mostafa, is that the lab can continually adjust still-shaky supply chains to acquire the assays and reagents needed to perform the tests. When supplies needed for one platform fall short, she works to get the materials from other companies.
"Supply chain issues continue to plague us, although we are in good shape with testing capacity given the redundancy we have established," says Carroll.
The original test developed by Carroll and Mostafa, which required manual rather than computer analysis, is still used in cases when sputum is collected from patients with a productive cough, she says.
For all testing, the sputum or nose swabs are delivered to the lab in the basement of the Johns Hopkins Hospital's Meyer building, where they are sorted by urgency. More than 7,000 one-hour "stat" tests have been conducted for time-sensitive situations, such as patients needing emergency surgery.
Clinical sensitivity can be difficult to determine, says Carroll, partly because no objective standard exists and because so many people with the coronavirus experience few or no symptoms. But Carroll and Mostafa believe their tests rarely if ever give false positives related to cross-reactivity with other viruses.
Posted in Health
Tagged johns hopkins hospital, coronavirus, covid-19