Peter Thielen and Tom Mehoke have spent years sequencing the genome of influenza. Now, as a new strain of coronavirus spreads across the globe, these biologists from Johns Hopkins Applied Physics Laboratory are transitioning their work to better understand the virus that causes COVID-19.
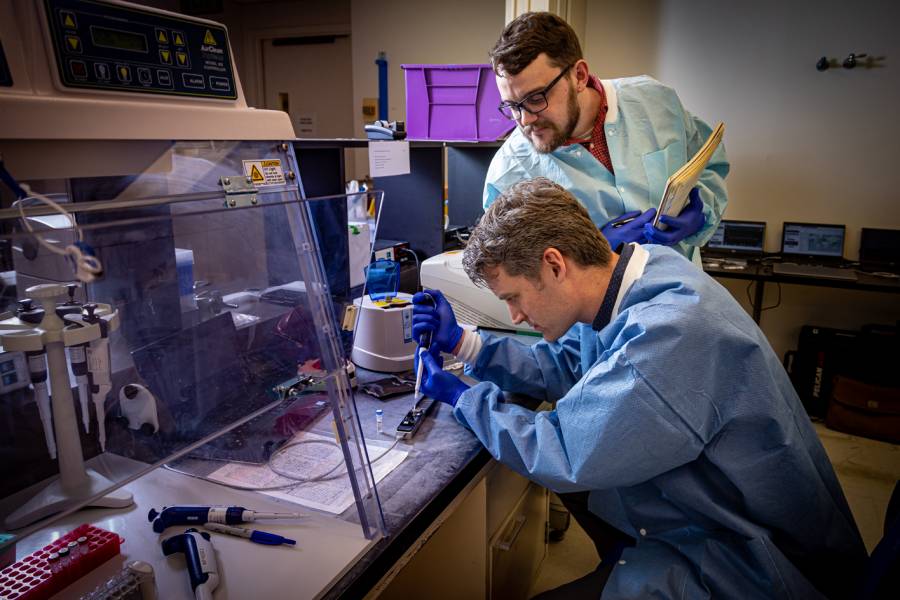
Inside the molecular diagnostics laboratory at Johns Hopkins Hospital, while health care workers and hospital staff work tirelessly to process patient tests, Thielen and Mehoke, members of APL's Research and Exploratory Development Department and the Johns Hopkins Center of Excellence in Influenza Research and Surveillance, are waiting for the positive tests. Certainly, positive tests are no cause for celebration, but for Thielen and Mehoke, they are a key to learning more about the rapidly spreading virus.
With software and molecular biology approaches developed in part at APL, Thielen and Mehoke are using handheld DNA sequencers to conduct immediate on-site genome sequencing of SARS-CoV-2—the virus that causes COVID-19.
"This information allows us to track the evolution of the virus," Thielen said. "It gives us a sense of where the new cases coming into Baltimore could've originated, and insight into how long transmission may have occurred undetected. There are a lot of things we can glean from that."
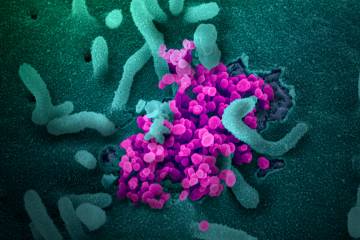
Topping that list is the ability to see how quickly the virus mutates—integral information for mapping its spread, as well as developing an effective vaccine. Influenza, for example, mutates constantly. That's why it's necessary to vaccinate against different strains of the flu each year.
The virus causing COVID-19, Thielen said, does not appear to be mutating as fast.
"When this virus was first sequenced in China, that information was helpful in starting the process to develop a vaccine," Thielen explained. "What we're doing informs whether or not the virus is mutating away from that original sequence, and how quickly. Based on the mutation rate, early data indicates that this would likely be a single vaccine rather than one that needs to be updated each year, like the flu shot."
In the near-term, the mutations inform how the virus is spreading.
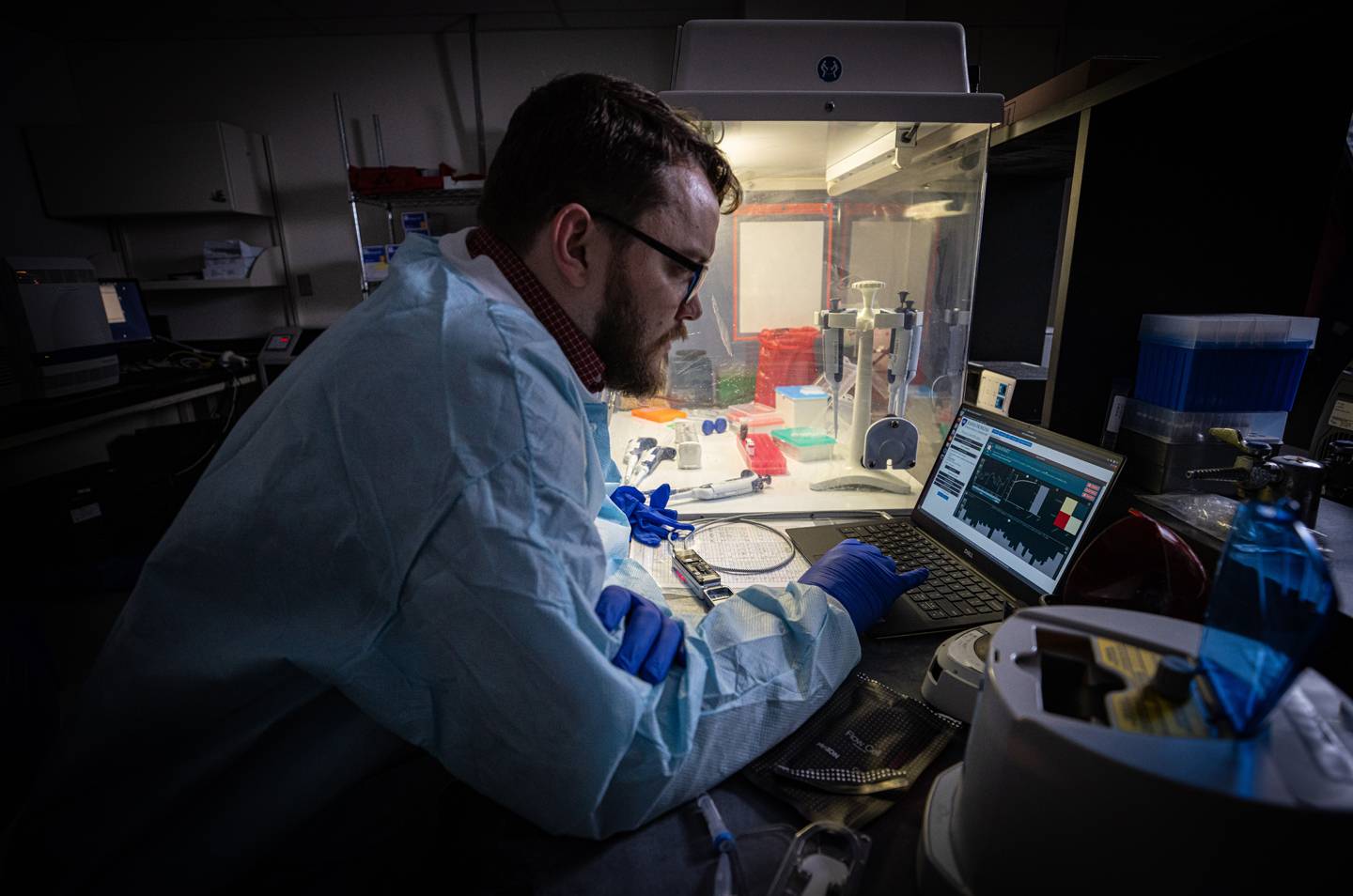
Image caption: APL biologist Tom Mehoke reviews the DNA sequencing analysis of SARS-CoV-2, the virus causing COVID-19, at the molecular diagnostics laboratory at Johns Hopkins Hospital.
Image credit: Johns Hopkins APL / Ed Whitman
With the United States continuing to ramp up testing and mitigation capabilities, the ability to understand how outbreaks are linked gives public health departments another tool for evaluation. Mutations can explain how long the virus may have gone undetected and the supposition that there are likely far more cases than diagnosed, and can advise on what measures to put in place (such as the social-distancing efforts and closings that are ongoing nationwide).
Sequencing of the virus' genome is being performed by scientists all over the globe as they work to trace the source of regional outbreaks. In northern California, for example, news reports suggest that genome sequencing has linked the Bay Area outbreak to the Grand Princess cruise ship, which linked back to the virus found in Washington State, which likely came from China.
That's the type of insight—a DNA fingerprint, if you will—that Thielen and Mehoke will gain as more virus genomes are sequenced from the Baltimore and Washington, D.C., regions.
They've completed analysis of the first four COVID-19 samples, with upward of 100 in the queue from the Baltimore/Washington, D.C. area, and expect many more in the coming weeks.
Operating remotely with handheld sequencers and laptop computers, Thielen and Mehoke's process required a several day wait before results could be transferred. But, at the end of last week they validated a new process that enables same-day sequencing—one that can be done by the hospital staff members already administering the diagnostic tests.
In the last nine months, Thielen and Mehoke held two workshops with the National Institutes of Health Fogarty International Center to help train scientists from low- and middle-income countries on how to use the handheld sequencers to do this work. The latest workshop was held virtually last week, when they trained stateside researchers to do the same type of on-site sequencing in their own laboratories.
"We were doing that to prepare as many researchers as we can, in the event that there would be a future pandemic," Thielen said. "It's here."
Posted in Health, Science+Technology
Tagged applied physics laboratory, genomics, apl, coronavirus