- Name
- Paulette Campbell
- Paulette.Campbell@jhuapl.edu
- Office phone
- 240-228-6792
A team of researchers from Johns Hopkins is leading the way in understanding how the advent of electronic medical records with large image databases and advances in artificial intelligence with deep learning can offer medical professionals new opportunities to dramatically improve disease diagnostics.
Researchers from the Johns Hopkins Applied Physics Laboratory and collaborators at the Johns Hopkins School of Medicine have developed image analysis and machine learning tools to detect age-related macular degeneration, or AMD, a condition that causes lesions on the part of the eye called the retina. When not detected early, the vision loss caused by the lesions is often irreversible. It is the leading cause of blindness in individuals over the age of 50.
The APL team partnered with researchers at the Johns Hopkins Wilmer Eye Institute on ways to automate AMD diagnosis, discovering that machine diagnostics using deep learning can match the performance of human ophthalmologists. The findings are published in JAMA Ophthalmology.
"We've been able to show the feasibility of automated fine-grained classification of AMD severity that only highly trained ophthalmologists can achieve," said APL's Philippe Burlina, a co-principal investigator for the project. "These techniques have the potential to provide individuals with automated grading of images to identify AMD or monitor those individuals with earlier stages of AMD for the onset of the more advanced stages when prompt treatment may be indicated to reduce the risk of blindness."
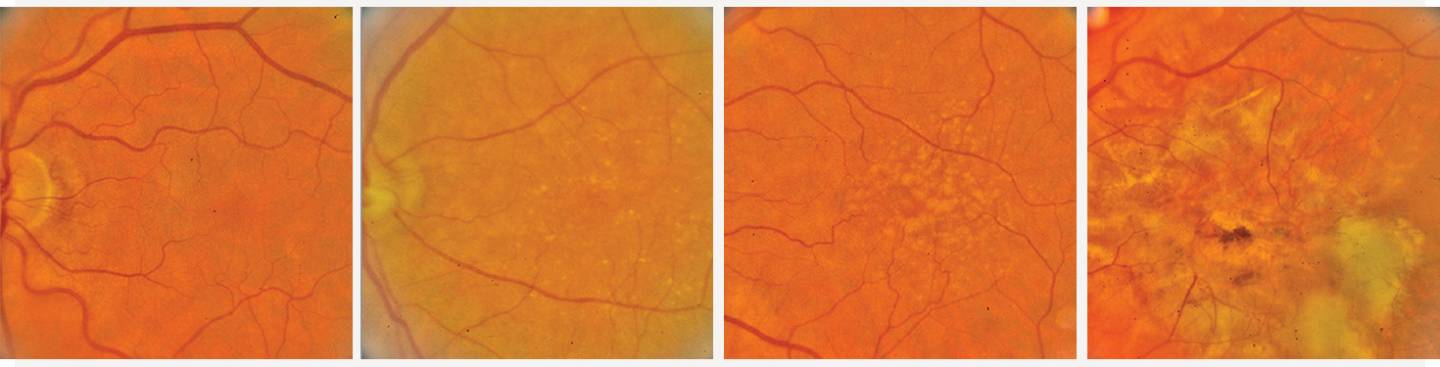
Image caption: Images show the progression of age-related macular degeneration: (from left) disease-free, early stage AMD, intermediate AMD, and advanced stage AMD
Image credit: Applied Physics Laboratory
The team has also expanded its inquiry to characterize layers of the retina during optical coherence tomography, or OCT, a noninvasive imaging technique that provides high-resolution, cross-sectional images of the retina, retinal nerve fiber layer, and optic nerve head. Such techniques can be used to diagnose other retinal diseases such as diabetic retinopathy and have the potential to help characterize vascular and neurodegenerative pathologies.
"We were able to show that machines can do as well as humans for diagnosing AMD," Burlina said. "So now we have started looking at other retinal diseases and how to combine images with other sources of information—demographics, lifestyle factors such as smoking, and sunlight exposure—to automatically perform prognosis and predict the probability for five-year risk of developing the advanced form of the disease. The end goal is to help clinicians and guide treatment."
This year, the team expanded its collaboration to include scientists from the Singapore National Eye Center and tested its algorithms on groups of individuals from Malaysia, India, and China. In a review for Nature Medicine, the team examines the potential of AI applied to retinal image diagnostics and discusses requirements and future work needed to allow translation and deployment of these techniques for clinical and point-of-care scenarios.
Burlina said the researchers will also work with hospitals in Thailand, Brazil, and France to explore how algorithms trained on a database of specific ethnicities, demographics, and imaging-capture scenarios can be adapted for different ethnicities and conditions.