A new five-year collaboration between Johns Hopkins University and biopharmaceutical company Bristol-Myers Squibb aims to determine why some patients being treated for cancer respond to immunotherapy drugs called checkpoint blockers and some do not, and to develop more effective combination immunotherapies.
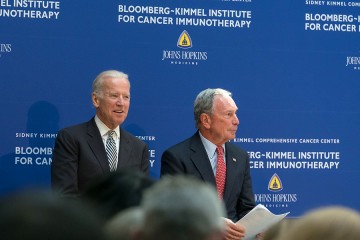
Projects included in the collaboration will span laboratory research on patients' tumor samples and several early-stage clinical trials led by Johns Hopkins scientists at the Bloomberg-Kimmel Institute for Cancer Immunotherapy.
"We're at an inflection point of understanding the root causes of response and resistance to immunotherapy, and this collaboration will help propel the research needed to identify ways to expand immunotherapy effectiveness to more patients," says Drew Pardoll, director of the Bloomberg-Kimmel Institute.
Under the agreement, scientists will focus on research aimed at revealing the ways cancer cells avoid or succumb to immune checkpoint-blocking drugs, which work by disrupting signaling systems used by cancers to avoid detection and destruction by immune cells.
One key system, say the Johns Hopkins scientists, provides a kind of "handshake" or connection between PD-1 receptors on immune cells and their sister-proteins, called PD-L1, on tumor cells. Anti-PD-1 checkpoint inhibitors block that handshake, which alerts immune cells to flock to cancer cells and target them for destruction. Between 15 and 65 percent of patients with melanoma; Hodgkin's lymphoma; and lung, kidney, bladder, and head and neck cancers respond to anti-PD-1 therapies, according to the scientists.
The scientists liken their research to canvassing a tumor's neighborhood, taking a closer look at the population of immune cells, the ways they signal each other and cancer cells, and how they move around.
Researchers at Johns Hopkins will explore identification of novel receptors or antigens on immune system T cells, tumor microenvironment interactions, and the role of the microbiome in therapy responsiveness.
Among the new technologies Johns Hopkins scientists will use is multispectral immunohistochemistry, which outlines the geography of immunological events inside a tumor before and after treatment with checkpoint-blocking drugs. The technology also allows scientists to map the expression of multiple proteins on individual cells, compared with traditional single-protein tracking methods.
The scientists plan to focus some of the clinical trials within the agreement on integrating immunotherapy into so-called neoadjuvant treatments, given to patients prior to their initial cancer surgery.
Officials at Johns Hopkins say the agreement builds on a fruitful track record of collaboration with Bristol-Myers Squibb and paves the way for additional industry-university research collaborations in immunotherapy and other cancer research areas.
Johns Hopkins is a founding member of the International Immuno-Oncology Network, a global collaboration among Bristol-Myers Squibb and 13 academic medical centers that aims to further the scientific understanding of immuno-oncology.