A team of Johns Hopkins students devised a system to improve the way lifesaving shocks are delivered to hearts earned first prize in the undergraduate division at the national Collegiate Inventors Competition.
In the graduate-level competition, Isaac Kinde, a Johns Hopkins medical student, received third-place honors for developing a test to detect ovarian and endometrial cancers.
Winners in the Collegiate Inventors Competition were announced Tuesday after the finalists presented their projects to contest judges at the U.S. Patent and Trademark Office in Alexandria, Va. This year's judging involved 31 students representing 13 entries—six undergraduate and seven graduate projects—from universities and colleges across the United States. After the judging, all finalists were invited to the White House to meet with John Holdren, a senior adviser to President Obama on science and technology.
The PrestoPatch system, developed by eight Johns Hopkins biomedical engineering students, took the top honor among the undergraduate teams. The system is designed to be used during the administration of electric shocks to patients experiencing arrhythmia, an erratic heartbeat that can be fatal. During this treatment, the doctor must decide where to place two electrode patches: on the front, side, or back of the patient. The electric current passes through the heart as it moves between the two electrodes. If the first shock doesn't work, current patches cannot be moved to a new position that may yield better results. But the PrestoPatch system allows the doctor to attach three patches to the patient, instead of two. If the first shock doesn't help, the doctor can quickly flip a switch and change the current's path through the body.
The system also addresses impedance, which occurs during defibrillation when the patient's body resists the lifesaving current. Doctors currently try to overcome this problem in a crude manner by pressing down on a patient's patch with their fists. To improve on this practice, the students devised a manual tool to apply the pressure in a standardized way. Lights on the tool alert the doctor when the proper pressure is applied.
"We were up against tough competition," said team leader Piyush Poddar of Plainsboro, N.J. Team member Sandya Subramanian of Grand Rapids, Mich., added, "There were a lot of projects that were technologically complex, but our device is simple. That means clinicians are more likely to use it."
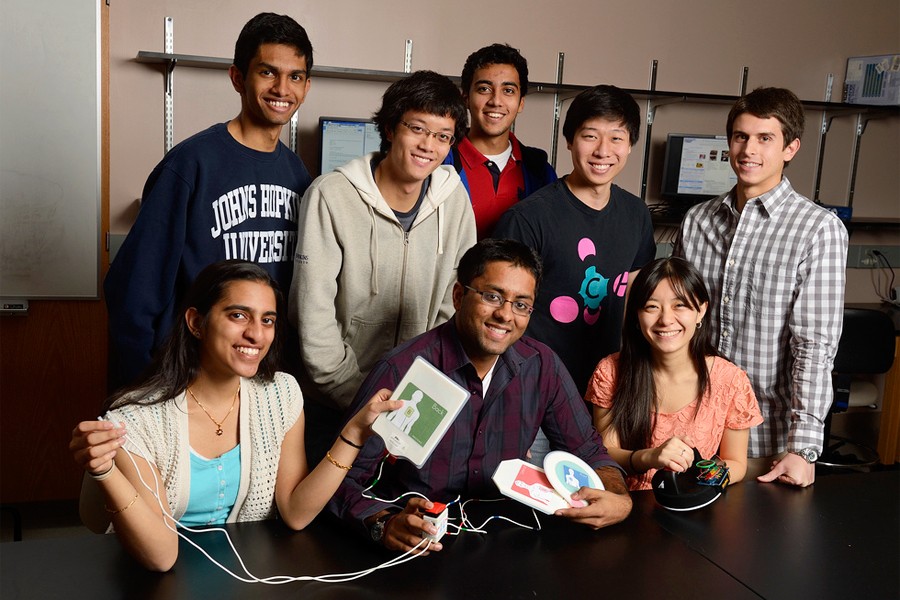
In addition to Poddar and Subramanian, the PrestoPatch team members are Aaron Chang of Grand Prairie, Texas; Kevin George of Acton, Mass.; Peter Malamas of Bucks County, Pa.; Melinda Chen of Baltimore; Rohil Malpani, of Kolkata, India; and Joon Eoh, of College Station, Texas. The team members said they plan to use their $12,500 in prize money to help launch a company aimed at moving their invention forward.
The team's project sponsor was Todd J. Cohen, who earned his undergraduate and medical degrees at Johns Hopkins and who now is director of electrophysiology at Winthrop University Hospital in Mineola, N.Y. The students' project emerged from the undergraduate design team program offered by the Department of Biomedical Engineering, which is shared by the university's schools of Medicine and Engineering. The work is conducted within the Center for Bioengineering Innovation and Design, known as CBID. The team's faculty adviser was Robert Allen.
This was the second consecutive year that a Johns Hopkins undergraduate biomedical engineering team finished first in its division. Last year's winners invented a device called FastStitch, a disposable suturing tool to guide the placement of stitches and guard against the accidental puncture of internal organs.
Kinde, who was honored in the graduate division of the inventors contest, used cervical fluid obtained during routine Pap tests in the development of the new test to detect ovarian and endometrial cancers. In a pilot study, the PapGene test, which relies on genomic sequencing of cancer-specific mutations, accurately detected all 24 (100 percent) of endometrial cancers and nine of 22 (41 percent) ovarian cancers.
Kinde, part of a research team at the Johns Hopkins Kimmel Cancer Center, and his colleagues say larger-scale studies are needed before clinical implementation can begin, but they believe the test has the potential to pioneer genomic-based cancer screening tests. Kinde's faculty adviser is Bert Vogelstein, professor of oncology and co-director of the Ludwig Center at Johns Hopkins.
A team from Stanford won the graduate student category with a molecular invention that dramatically enhances the ability of the body's immune system to kill cancer cells.
Posted in Science+Technology, Student Life
Tagged undergraduate research