It's hot. The sun bakes the red rocks and sandy mesas of Tuba City—known to locals as "Tuba"—but that's hardly a reason to stay home, especially today. It's homecoming weekend for the local high school, and the flea market is out of pandemic hibernation. In advance of the parade and big game, hundreds of residents of the Navajo Nation have come to browse bolo ties, eat slices of melon, and exchange friendly jibes with their neighbors. "You should be wearing green!" one old man yells to another. Many are donning the color of the Tuba City Warriors as they amble past artisans offering beadwork, spices, and fry bread.
The turnout is not only a good thing for the vendors; it may also benefit science. Nestled among the maze of stalls are two tables staffed by workers from the Johns Hopkins Center for American Indian Health. (Editor's note: The center changed its name to the Center for Indigenous Health in September 2022.) They're here to recruit participants for a dizzying array of programs that all share one aim: elevating the health status of Native Americans.
Among them is Stacey Robbins, a family health coach for a program called Asdzáán Be'eena' (in English, Female Pathways) that aims to curb high-risk behaviors and increase cultural connectedness among Indigenous girls through education (e.g., how to say no) and strengthen bonds with a female caregiver. An auntie approaches the booth and Robbins tells her about the program, including how it incorporates traditional Diné, or Navajo, teachings, such as using running as a form of prayer. The auntie likes the sound of it—her niece might be interested, too, she says—and gives Robbins her details. "We're trying to catch these girls at a young age and break the cycle," Robbins, who is Diné, tells me.
The "cycle" is not a single thing. Generational challenges range from young motherhood—American Indian and Alaska Native women are more likely than any other race to give birth in their teens, according to the Centers for Disease Control and Prevention—to the outsize proportion of Indigenous people who are killed in motor vehicle crashes: Among children, the death rate is up to six times that of other ethnicities. High school students living on reservations report early and higher-than-average use of alcohol, cigarettes, and illicit drugs. Indigenous adults are twice as likely as whites to be diagnosed with diabetes. And the suicide rate among Indigenous people is stubbornly high, today more than 3.5 times higher than that of the lowest-risk groups.
Standing near Robbins, under a blue tarp shielding the workers from the sun, is Jennifer Richards, an assistant scientist at the center who grew up in Tuba. She loved much of that life—the stark and stunning land, the way neighbors helped raise one another's kids—but she also witnessed firsthand the statistical disparities. "There were people who died in car accidents. It wasn't abnormal to hear of relatives losing their limbs or going blind because of diabetes. I had a friend who took their life," Richards says. "I just knew a lot of my relatives didn't have to go through these illnesses and early death." That revelation was the seed of her passion in public health, the art and science at the heart of the center's work.
The center just marked its 30th anniversary, a milestone that comes at a time of explosive growth. In the past two years, the center's staff has nearly doubled, from 130 to more than 250, and so has its budget, from $12 million to more than $22 million. In response to the pandemic, institutions and philanthropic individuals opened their wallets, wanting to funnel money where it would help most. While its work is varied today, the center began with research on infectious disease that has helped shift standards of care around the U.S. and the world and saved millions of lives. On top of that, widespread media coverage made it clear that the population the center aims to help was being disproportionately hurt by COVID-19. A study published in February indicated that Indigenous people were dying at almost twice the rate of whites.
"These [past] 18 months, more Americans have paid attention to the plight of Native Americans than probably ever before in our modern history," says Allison Barlow, who has been with the center since 1991 and was named director in 2016. "The reason [COVID-19] hit tribal communities so hard is because of the injustices that have been dealt to them since colonization." Wrenching stories documented the threat to elders, precious protectors of Indigenous ways. It became clear that they could go away, that the culture could be lost. "And it was this wake-up call," Barlow says, "about this sacred treasure within our borders that's so easy to just ignore, forget, neglect."
With a spotlight trained on Indigenous people and money to spend, the center's team hasn't been idle. In addition to helping with the COVID-19 response and expanding existing programs to interested tribes around the country, center staff are working to increase support for Indigenous scholars who can be the next generation of experts in public health. Barlow also hopes this will be a moment when outsiders will take note of the wisdom tribes are displaying, as many Indigenous people willingly take vaccines to protect the most vulnerable among them. The pandemic, Barlow says, has provided "this window into seeing the intelligence of their value system."
The Center for American Indian Health's origin story begins half a century ago and half a world away, when a young man named Mathuram Santosham was a medical student in India. It was the late 1960s and seemingly every day Santosham was watching children die from dehydration caused by diarrhea, often a result of contaminated water or food. At the time, the standard of care was to give people lifesaving fluids through an IV. But once they were sick, many children couldn't get to a hospital. And even if they did, there might not be enough tubing or fluids or trained personnel to treat them.
"Moms would pull on my coat and say, 'Come help my kid,'" Santosham recalls. "And by the time I'd get there, that kid would be dead." He resolved to find another way.
After medical school, Santosham—who led the center until 2016—went to the U.S. for additional training and eventually began working alongside two researchers at Johns Hopkins who were breaking ground with a potentially revolutionary solution: oral rehydration. If scientists could determine the right mixture of sugar and salts, the idea held, then people could mix up replacement fluids right at home like a cup of Gatorade.
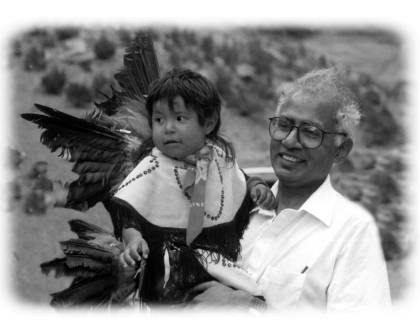
Image caption: Mathuram Santosham
Image credit: Courtesy of the Center for American Indian Health
Santosham, who studied under Harold Harrison and Bradley Sack, prepared to head back to India for further research. But as he and his wife readied to buy their tickets, conflict broke out between India and Pakistan, and those plans were abruptly scuttled. One of Santosham's mentors suggested an alternative that would shape the course of his life. Sack was preparing to start a five-year oral rehydration study with another population that suffered from poverty, lack of infrastructure, and high rates of death: the White Mountain Apache Tribe, whose reservation lay in the high forests of Arizona.
When he arrived, the young doctor was again faced with horrific scenes. "I was absolutely shocked," he says of how many White Mountain Apache children were dying from dehydration. But once the project started, the story changed. Santosham trained local community health workers to distribute his team's solution—a packet of dry ingredients designed to be mixed with one liter of water—and educate parents on how to use it. "The deaths just came down dramatically," he says. The results of that project, along with others, helped scale oral rehydration as the standard of care around the world, a shift that has saved an estimated 50 million lives in the past four decades. The work also inspired the now ubiquitous hydration product Pedialyte.
Other revelations soon followed, such as the prevalence of meningitis, inflammation of the membranes around the brain and spinal cord that can be life-threatening. During trials for the oral rehydration solution, Santosham noticed that meningitis had an attack rate in the White Mountain Apache community that was about 100 times the national average. The source appeared to be a bacterial infection called Haemophilus influenzae type B, also known as Hib. Almost all the cases on the reservation were happening in children less than a year old, and at the time, there was no Hib vaccine available for children that age. Over the next decade, Santosham researched and tested new candidates until he found one that worked effectively for both the White Mountain Apache and Navajo communities.
Today, the CDC recommends that children get their first Hib vaccine at 2 months old, a guideline that has roots in the partnership between Johns Hopkins and the White Mountain Apache Tribe. In fact, says Barlow, three of the eight vaccines that are now routinely given to children in their first nine months of life—Hib, rotavirus, and pneumococcal—were first proved effective in tribal communities by the center's researchers. It is a case of medicine pioneered by grave need.
Such discoveries were only possible because tribes were willing to participate. And that was only possible because Santosham, known to friends as Mathu, earned their trust. He consulted tribal leaders before he began, was responsive to their needs, attended three-daylong wakes, and drove a bus around the reservation to take kids to Sunday school. That bond is the foundation upon which the center was founded in 1991 and remains a defining feature today.
"[Johns Hopkins researchers] don't just show up and say, 'I'd like to do this. Listen to me. This is best for you,'" says Loretta Christensen, a member of the Navajo Nation and the chief medical officer for the Indian Health Service. "They understand the culture of each place they work. They respect it, and they work with it."
That might mean consulting traditional healers as they work on health initiatives, employing people who speak native languages, or switching gears when tribal councils alert them to new needs. Today, the center has outposts in New Mexico, Arizona, and the Great Lakes region, reaching a total of more than 150 tribal communities.
That combination of trust and the center's history with infectious disease made it "uncannily ready" to respond to the COVID-19 pandemic, Barlow says. Before there was an official pandemic, public health experts knew that the communities were high-risk, given multigenerational households and lack of running water, to name just two risk factors. And in the months following the World Health Organization's pronouncement that we were, in fact, in a pandemic, those fears were borne out. Data suggested that Indigenous people were being hospitalized and dying at higher rates than those who lived beyond reservation borders. By May 2020, the Navajo Nation had surpassed New York in having the highest per capita coronavirus infection rate in the country.
Many tribes, aware of the tsunami coming, were quick to close their borders and order people to shelter in place. In Whiteriver, Arizona, where Santosham's work began, emergency orders came on March 12, 2020, one day after the WHO's declaration. The first positive case on the reservation was documented April 1 and the spread was quick. It wasn't long before the center's employees were routinely working 16-hour days on COVID-19 relief.
The center quickly developed testing and data-tracking systems to be used in Indian Country and worked with the Indian Health Service to spread reliable information. Researchers helped interested tribal members volunteer for Pfizer's vaccine trials and ran those trials in the Navajo and White Mountain Apache communities. Armies of employees sourced personal protective equipment and cleaning supplies and literal tons of food and water, then assembled and delivered supply boxes for families who had to quarantine. Workers delivered medicine and mail. Employees built handwashing stations in the Navajo Nation, where an estimated 30% or more of households don't have running water. On the Fort Apache reservation, they connected sick people with the hospital and checked in daily on tribal elders.
"We were their counselors and therapists," says Ryan Grass, a senior research program coordinator at Whiteriver. People were starved for human interaction. Some families would break down during their visits. "When we dropped stuff off," Grass says, "they would talk to us for hours."
The center also helped run "testing blitzes" and, later, "vaccine blitzes." They used grant money to put on virtual town halls and film public service announcements that featured leaders, including traditional healers, who could explain why getting vaccinated was such an effective way to fight the "monster," as many Diné have come to call COVID-19. And they used other newfound funding to hire tribal members to do relief work in their own communities, where seemingly everyone knows someone who died from the virus. "We all lost somebody," Richards says.
But out of the trauma also came inspiring action. What makes the center particular, Richards says, is that it operates with the understanding that there are unique "Indigenous determinants of health." Some of these, like racism and geographic isolation, are challenges. But others, like tribal sovereignty and collective spirit, are assets. Tribal leaders in places like the Navajo Nation imposed strict curfews, mask mandates, and social distancing requirements. And people complied, in part because of their traditional reverence for the oldest and youngest among them. As tribal people proved less susceptible to misinformation and more willing to take a vaccine, the curve flattened. As of print time, nearly 70% of eligible people in the Navajo Nation had been vaccinated. Nationwide, the rate was less than 60%.
In the late 1980s, the White Mountain Apache and Navajo tribes told Santosham they needed a different kind of help. "It's great you're working on all these infectious diseases," Santosham recalls tribal leaders saying, "but we have other problems." Diabetes. Obesity. Psychological stress. Santosham, a pediatrician, wasn't equipped to tackle them all. He turned to the then dean of the Johns Hopkins School of Public Health, Donald Henderson—an epidemiologist who helped eradicate smallpox—and Henderson, along with Santosham's department chair Robert Black, suggested starting a hub that could draw on expertise from across the university. This led to the center's formation and a second arm of work in mental and behavioral health that has since yielded dozens of studies and programs, focusing on everything from healthy eating to toxic masculinity. A special focus has been suicide.

Image caption: Mathuram Santosham
Image credit: Courtesy of the Center for American Indian Health
Underlying the center's approach is the belief that current plagues are inextricable from historical trauma. "The forced relocation that our people experienced, whether that was boarding school or acts of genocide or land theft, disrupted that connection to land, disrupted Indigenous parenting and cultural teachings," Richards says. "And that has manifested through the generations into some of the disparities we're seeing today." This is why culture revitalization is woven into nearly everything the center does.
Take high rates of diabetes. From the center's point of view, this disparity has roots in the American government's systematic killing of bison that Indigenous people relied on and their displacement from fertile earth to barren land. Over time such injustices have morphed into problems like food deserts. The Navajo Nation, for example, is the size of West Virginia and boasts a mere 13 grocery stores. Combine that with high rates of poverty, and it is clear why many people end up relying on gas stations for food. Today, the center's educational interventions with families might include advice like minimizing sugary drinks and the importance of balance.
The connection between physical and cultural struggle is clear to people like Joe Baca, a 46-year-old social worker who is participating in a pilot program in Tuba City called Azhe'é Bidziil (in English, Strong Fathers), which covers not only such issues as parenting strategies, financial planning, and domestic violence prevention but also history. "A lot of us men, we struggle along the way, and that can be for many reasons," says Baca, a father of two who has been sober for 16 years. Drugs. Violence. Unstable households. Sometimes, Baca says, those problems have been passed down from generation to generation, starting with a relative who endured suffering that "essentially just ate them alive."
It's a cloudy day in late September, and employees on the Fort Apache reservation are settling into a new office, a double-wide gray trailer added to contain "overspill" from the center's recent growth. The phone lines aren't up yet, so Novalene Goklish is directing her team through a walkie-talkie. Behind her on the wall hangs a sign that says, "Sarcasm Welcome." This is the command center from which she and her team are overseeing more than 15 programs related to mental and behavioral health that serve some 13,000 people on the reservation plus other tribal members in the surrounding 60-mile radius. Across the road, in another trailer, is a Johns Hopkins infectious disease team.
Goklish, a senior research associate who is a member of the White Mountain Apache Tribe and grew up here, has been with the center for nearly 25 years. Sitting across from her is fellow senior research associate Francene Larzelere. She has been an employee for more than 17 years but first encountered the center years before as a participant in a program that aimed to empower young mothers. The center's ties run deep.

Image caption: Director Allison Barlow (center) with senior research associates Francene Larzelere (left) and Novalene Goklish, both White Mountain Apache, at the Center for American Indian Health’s location in Fort Apache, Arizona.
Image credit: Ed Cunicelli
More than one of the programs Goklish and Larzelere oversee tie back, in overt and subtle ways, to an epidemic of suicide that has plagued the community for decades. In 2019, the CDC released an analysis showing that in the U.S. overall, the suicide rate was up 33% since 1999. But for Native American women and men, the numbers were far worse: 139% and 71%, respectively. "Growing up, you're taught not to talk about suicide, think about it, because you're inviting negativity and bad spirits into your life," Goklish says. While that doesn't make the scourge go away, it can make it hard to address.
The center's foundational program, developed through a partnership with the tribe, is called Celebrating Life, and there is not another one like it in the country, Barlow says. The name reflects advice that Goklish and her team got from tribal elders, whom they brought in many years ago when they were struggling to overcome the taboo around the act. "We learned from our elders that we needed to focus on the life side," Goklish says. "[Make sure they know] that we value them as a community member, tribal member, and family member."
The unusual part of this intervention is that officials at every agency, from law enforcement to the emergency room, are required by law to report suicidal behavior, whether a person has attempted it or has been binge drinking in a way that could be related. Those reports all go into a system that is run by the center, and someone from their team is assigned to go check on that person and follow up for as long as is needed. On that first visit, the employee might just talk to them or offer an adult coloring book to help occupy the person's mind. Sometimes, Goklish says, they take the person for a drive to a river that goes through town just so they can listen to the water and maybe find some peace. They might also take them to the ER.
Sometimes they stay the whole day. "There's no time cap," Goklish says. "Maybe they [tried to hang] themselves three days ago, and now we are the first one to show up. When they're talking to us, we want to make sure that we're there for them, you know, we're not there just to gather data."
Follow-up might include helping them get an ID so they can apply for some type of aid or helping them return to school. As awareness of the program has grown, referrals have increased from about 200 a year to 2,000 a year. The approach has been lauded by institutions such as the American Psychiatric Association.
Other programs aim to mentally and emotionally strengthen tribe members, which could help prevent dark outcomes years down the line. One example: bringing tribal elders into schools, where they give lessons in both English and Apache. They might show kids artifacts like cradleboards, used in a time when families on the reservation lived in shelters made from grass and branches. They teach them about clans and encourage kids to figure out which clans they belong to. Practically, this system helps relatives avoid intermarriage, but it can also help someone develop a sense of self.
One of these elders is Evelyn Massey. When asked for her age, she laughs and says "18 backwards." During our interview at the Whiteriver office, she often turns to a center employee sitting with us and asks for clarifications in Apache. I ask what she would highlight from her lessons. Massey says it boils down to teaching children "what we went through, what we know, how we will survive." Part of this is learning the Apache language, one classified as "threatened" by the Endangered Languages Project. Massey links suicide to young people not having enough confidence in who they are. "They need to belong," she says. "They need an identity."
In the early 2000s, the center's leadership received an $8 million bequest and used it to launch a third arm dedicated to training Indigenous scholars—a kind of academic gateway that could both empower people to lead public health efforts in their own communities and help get them a seat at the table where big decisions were being made.
The importance of the latter aim is exemplified in a 2018 report from the U.S. Commission on Civil Rights titled "Broken Promises," which details myriad ways the American government has failed to live up to the assurances it made to tribes in 375 treaties. It connects these failures to the fact that Native Americans continue to rank near the bottom of all Americans in health, education, and employment. One reason for those failures is that Congress, which welcomed its first Native American women just three years ago, has repeatedly failed to provide adequate funding for necessities ranging from infrastructure and housing to economic development.
Santosham, who at age 77 is now the director emeritus of the center, recently bought a summer home near the Fort Apache reservation, where children he cared for now have their own kids and, in some cases, grandkids. Speaking to me from that home in Lakeside, Arizona, he proudly recounts how far the center has come. "I kept thinking, the problems will never go away with just outsiders coming in," he says. "If you're going to make a real difference, local people have to take charge." In the past two decades, the center has helped scores of Indigenous people get an advanced degree. Many have gotten their PhDs. And thousands have gone through a certification program the center offers that provides a public health education through an "Indigenous lens."
One of those graduates is Joshuaa D. Allison-Burbank, who grew up in Tohatchi, New Mexico, on the Navajo Nation. He did the certificate program while completing his PhD in speech language pathology at the University of Kansas and took a hard turn from planning to be a clinician to working in public health. "I started realizing that in the time it took me to see a couple of kids in clinic, there was an opportunity to be serving an entire community," he says.
After working for the Indian Health Service, Allison-Burbank was recently hired by the center to work on a new program called Project Safe Schools. Focused on helping children safely get back into the classroom in the wake of COVID-19, its investigators are tackling medical issues, like how to do effective pooled testing, as well as social ones, like how to measure the burdens children are carrying with them after a year of isolation and struggle.
In addition to working on Project Safe Schools, Allison-Burbank is leading a new effort he conceived called Language Is Medicine. His idea was to incorporate Native language into the center's home visits, using them to strengthen family bonds—which, in turn, could help strengthen the languages too. The seed for this idea came when he was working on his PhD, as he watched how a language revitalization effort among the Potawatomi people in Kansas invigorated children and adults, establishing connections in an instant and making people feel pride in who they are.
"If someone doesn't know their language, they have limited ties to their culture and their community. And that is one major contributor to poor health," he says. "So how do we address that?" You bring the language back, lifting up the words that a previous generation was punished for speaking after they were forced to attend boarding schools designed to assimilate them into white society.
In linguistics, there is a theory known as the Sapir-Whorf hypothesis. It suggests, essentially, that an individual's thoughts and actions are limited by the language they speak, the words they know. Allison-Burbank notes that there is a word in Diné Bizaad (the Navajo language), hayoołkááł, that refers to the time of day that stretches to the cusp of dawn when there is a soft, gradual exchange between day and night. "That's one of our most sacred times of day," he says. "And unless you know the word or concept, you can't truly experience it." You cannot draw vigor from it. You cannot share it with others.
In many ways, Allison-Burbank and his colleagues see answers for the future in the past. Over the summer, as people struggled to get food, he noticed that his neighbors in the Navajo Nation were returning to traditional farming methods. The crisis was helping them return to the earth and restore a connection to the land that was systematically dismantled centuries ago. "In times of stress Native people survive," Allison-Burbank says, "because they go back to these resilient ways."
Posted in Health
Tagged public health, american indians, indigenous peoples day, covid-19








