When Jack Iwashyna was a new internal medicine resident working in an intensive care unit, he found that patients and their families often asked questions for which he was unprepared—questions about not just whether their loved one would survive, but also what their life would look like if they got out of the ICU.
Would they still be able to play with their grandchildren? How much time would they have to spend in a rehabilitation clinic? How independent would they be able to be?
"There were no data to answer them," Iwashyna recalls. "At the time, much of critical care medicine used inpatient mortality as its only outcome—either you died, or you were discharged alive. The prevailing narrative was that either patients died or they got better. I just didn't buy that."
When Iwashyna began examining what happens to patients after they are released from the ICU, he found that lasting impacts were quite common. Driven by an increasing conviction that the distinction between social programs and health programs was unproductive, he has since dedicated his career to finding ways to think about social and health safety net integration for patients to improve long-term health outcomes.
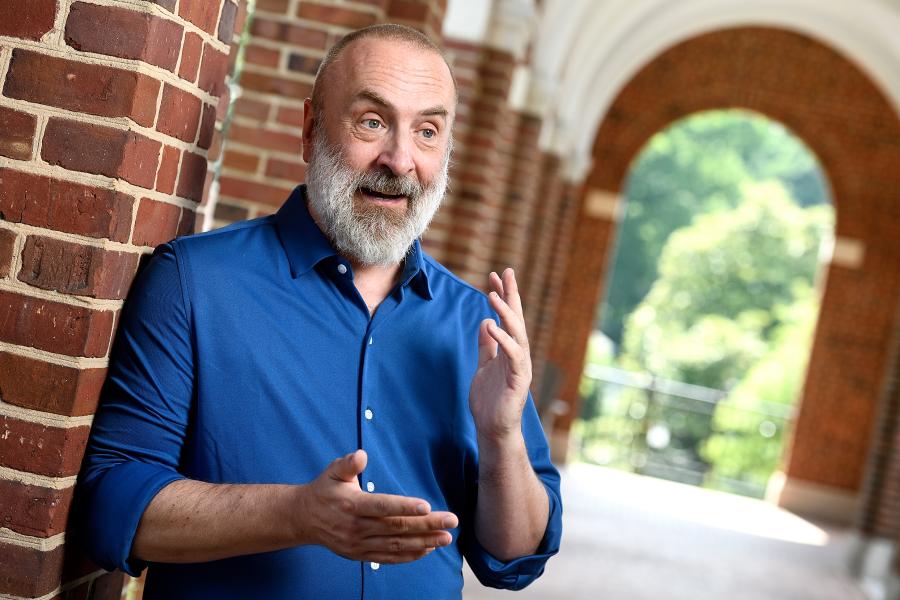
Iwashyna joins Johns Hopkins University as a Bloomberg Distinguished Professor of Social Science and Justice in Medicine. He holds primary appointments in the Division of Pulmonary and Critical Care Medicine in the School of Medicine and the Department of Health Policy and Management in the Bloomberg School of Public Health. He is also part of the Knowledge to Action and the Business of Health cluster, part of the second phase of the BDP program, which will double the total number of Bloomberg Distinguished Professors to 100. These faculty-developed interdisciplinary clusters will recruit new BDPs and junior faculty members to Johns Hopkins to conduct transformational research in 10 crucial fields.
A shift in focus
The combination of intellectual curiosity and desire for effecting change has been a guiding thread through much of Iwashyna's life. Early in his academic career as a pre-med student, a friend recommended he read William Julius Wilson's The Truly Disadvantaged and Douglas Massey and Nancy Denton's American Apartheid. There he found the logic and scientific rigor he enjoyed in his molecular biology studies applied to systemic racism and equity, issues he felt passionate about. The books inspired a shift in his academic focus—he added health policy courses in addition to neuroscience studies and would go on in graduate school to study questions such as how neighborhood segregation or integration impacted the provision of bystander CPR, or why people who are married tend to live longer.
Iwashyna, now a critical care physician and health services researcher, aims to improve health outcomes and quality of life for survivors of critical illness. He is interested in the ways in which a patient's environment influences the effectiveness of the care that a patient receives, as well as how critical illness impacts the patient's life course. His innovative research has provided evidence of the long-term impact of severe acute infections in the United States, showing that patients who survive sepsis often have enduring cognitive and functional deficits that last for years and result in difficulties completing basic activities in daily living, and that survivors are at higher risk for re-admission to the hospital and death.
Iwashyna has worked with an international coalition to reframe advice on inpatient treatment of sepsis to incorporate explicit discussions of supporting family members and including neighborhood context and financial resources as key components in recovery, as well as to redefine recovery not just as the absence of death, but rather as care to minimize risks of long-term disability and that considers the patient's wishes and personal values.
"My social science background helped me hear these conversations in the ICU and learn from them," Iwashyna says. "And my medical background let me hear them in a way that's biologically nuanced and have the urgency to meet them. And then social science helps me address them."
Inequity in COVID-19 care
This combination of areas of expertise and his methodological and clinical credibility proved immensely valuable as Iwashyna and colleagues rebuilt their hospital structure during the initial outbreak of COVID-19. Iwashyna helped stand up the COVID-19 unit at the University of Michigan and the Department of Veteran Affairs Ann Arbor Healthcare System, developing and co-leading a governance structure for implementing scarce resource allocation and working with engineers to assess the clinician safety of various oxygen delivery devices, in addition to treating patients in the ICU.
"With COVID-19, it became obvious pretty early on that we were making the same mistakes that we had made with other diseases, in that we were gathering statistics on whether a patient died or was discharged from the hospital," explains Iwashyna. "We had to pivot and ask not just if someone survived an initial hospitalization with COVID-19, but also: Did they come back to the hospital? Were they left with a disability? Are they losing their jobs?"
Iwashyna and his team demonstrated a high burden of readmission and mortality in COVID-19 patients that had been discharged from the hospital, as well as large and persistent disability, cardiopulmonary symptoms, and financial toxicity—the negative impact medical expenses can have on patients. He currently is working on identifying modifiable social and contextual factors that shape functional recovery after serious illness, and investigating the roles of employment, financial toxicity, and caregiver burden as both outcomes of and contributors to recovery. Iwashyna emphasizes the foundational role that Hopkins has long played in studying and improving such outcomes after critical illness, and the appeal of working on the topic with the paradigm-changing young clinicians and scientists already here.
COVID-19 showed how hospitals were repeating unjust patterns of care. Iwashyna argued in The New York Times in the fall of 2020 that large academic medical centers had an opportunity and moral obligation to find ways to centralize the care of COVID-19 patients with acute respiratory failure to save more lives. He wrote that doing so was a way to enact the commitments to equity that many institutions were espousing at the time.
COVID-19 also revealed ways in which systemic racism is baked into not just hospital systems, but the very technology used to care for patients with respiratory failure. Iwashyna and his team exposed evidence that pulse oximeters—a vital tool in assessing whether patients are getting enough oxygen into their blood and thereby also measuring COVID severity—showed consistent racial bias, failing to alarm when Black patients were not getting enough oxygen.
Iwashyna says that the work he has done on pulse oximetry is only possible because of the work of his talented mentees and draws on a long line of health disparities and social science research, much of it pioneered at Johns Hopkins. Part of what drew him to JHU is the work of young scholars examining racial bias and noise in pulse oximeters within the Precision Medicine program. In light of increased interest in the topic at the Food and Drug Administration—which convened an all-day panel on pulse oximetry bias in November 2022—Iwashyna is already working with a multidisciplinary team at Johns Hopkins to define standards that would allow institutions to evaluate the degree of equitable functioning of medical devices before purchasing them.
"Hopkins seems like an ideal place to find solutions to the specific problems of bias in pulse oximetry," he says, "but also the more general problem of detecting, regulating, and mitigating inequity in increasingly ubiquitous medical devices, algorithms, and diagnostic aids."
Thinking across disciplines
Iwashyna comes to Hopkins from the University of Michigan School of Medicine, where he was a professor of internal medicine, director of health services research, and co-director of the research core of the Center for Clinical Management Research at the Veteran's Administration Ann Arbor Healthcare System. While at Michigan, Iwashyna also co-directed the Michigan National Clinician Scholar Program, which takes clinicians from diverse backgrounds and provides them with rigorous research training for social change and encourages innovative thinking.
Iwashyna earned a bachelor's degree in molecular biology from Princeton University, a PhD from the Harris Graduate School of Public Policy at the University of Chicago, and an MD from the University of Chicago. He completed an internal medicine residency and a fellowship in pulmonary and critical care medicine at the University of Pennsylvania before joining the faculty in pulmonary/critical care at the University of Michigan School of Medicine.
At Johns Hopkins, Iwashyna hopes to build on his extensive teaching and mentoring experience, teaching talented young researchers to use the tools of social science and epidemiology to solve important problems in acute serious illness. He also hopes to pass on his interdisciplinary thinking and approach to the next generation of students in the School of Medicine working on innovative research in health services research by bringing them to other parts of the university to tap into the resources and knowledge existing in Baltimore.
"Simply put, Johns Hopkins gets the best raw young talent in the world coming as trainees," Iwashyna says. "Through the Bloomberg Distinguished Professorship, I will be able to work across schools and departments to support truly innovative new work in health services research. My goal is to build microenvironments around the students where they can thrive in these incredibly creative juices combined from the rich sources available to them at Johns Hopkins. If they can stay rooted in specific clinical problems and pull knowledge and tools from other fields, they will become uniquely positioned to answer questions that nobody else knows how to ask. And hopefully, to do this in a way that also asks 'how does this help us overcome the historical and ongoing racism in the medical system?'"
Iwashyna says he looks forward to being in an environment that facilitates thinking across disciplinary boundaries, and that has the knowledge and the resources to carry out large-scale studies as well as policy partnerships to be able to effect real change in the world.
"The distinctive institutional framework of the BDP program and of this cluster structure is that it creates a wide network of brilliant researchers to learn from and collaborate with that would otherwise take much longer to find and build up," Iwashyna says. "Working within this cluster will elevate my research and make it easier to discover and connect with folks across Johns Hopkins University."
"We are excited to welcome Jack Iwashyna as the next Bloomberg Distinguished Professor and a member of the Knowledge to Action and the Business of Health BDP cluster," JHU Provost Sunil Kumar says. "As an interdisciplinary researcher with a commitment to social justice in medicine, he will connect with colleagues across Johns Hopkins and make valuable contributions to the cluster's research direction. As a teacher and mentor, he will be instrumental in shaping the way that young scientists and physicians think about the intersection of critical care and social science."
"The BDP program encourages creative, collaborative thinking to solve some of the most vexing problems," says Theodore DeWeese, interim dean of the Johns Hopkins University School of Medicine and interim CEO of Johns Hopkins Medicine. "Jack Iwashyna's career has embodied exactly that same spirit. For decades, his work has challenged the status quo in his field of pulmonary medicine, always with the goal of improving the treatment outcomes for patients. He's an important voice in many of the most pressing conversations in medicine and we are lucky that he is part of Johns Hopkins. I'm excited to follow Dr. Iwashyna's research as he begins this new role as a Bloomberg Distinguished Professor."
"Dr. Iwashyna brings remarkable vision, drive, and experience to the Bloomberg School of Public Health," adds Ellen J. MacKenzie, dean of the Bloomberg School. "Throughout his career, he has asked tough questions about the realities of medical care, forged new paths in research, and worked continually to improve health outcomes and health equity. As a Bloomberg Distinguished Professor, I know he will build strong partnerships across our institution and make a powerful impact on the future of health policy."
As a Bloomberg Distinguished Professor, Iwashyna joins an interdisciplinary cohort of scholars working to address major world problems and teach the next generation. The program is backed by a gift from Michael R. Bloomberg, a Johns Hopkins alumnus, founder of Bloomberg LP and Bloomberg Philanthropies, World Health Organization Global Ambassador for Noncommunicable Diseases and Injuries, and 108th mayor of New York City.
Posted in Health, Science+Technology
Tagged health disparities, bloomberg distinguished professorships