Jessica Gill's mind is on the move.
A second ago, mired in scientific jargon, she was dropping names of biomarkers associated with brain activity, injury, and disease: proteins like GFAP, SNAP-25, NECAB1&2.
Then Gill's focus pivots. Her synapses fire; neurons bob and weave. Suddenly she's mentioning her kids—Portia and Teddy—while pulling up her phone's screensaver to show two teens, both sporting shiny smiles.
These, says Gill, Nurs '07 (PhD), are faces of traumatic brain injury (TBI).
Who? What? Let's slow down.
In addition to being Portia and Teddy's mother, Gill was the first nurse ever to win the prestigious Lasker Clinical Research Scholar Award from the National Institutes of Health. Her current professional title, Johns Hopkins Bloomberg Distinguished Professor of Trauma Recovery Biomarkers, is a mouthful, but apt. In a basement laboratory in the School of Nursing, she leads a team at the frontier of TBI research. Specifically, they are employing a gleaming new technology known as OLINK that can quickly detect and measure a mindboggling 5,400 proteins (GFAP and more!) present in bodily fluids— potential biomarkers that can indicate and predict diseases and disorders, including TBI.
Cutting back now to Portia and Teddy:
She is 18, a cheerleader. He, 14, plays football. Portia needed hospital care for TBI after a squad mate fell on her and they hit the ground hard, Gill recalls. And given Teddy's penchant for contact sports, it's hardly surprising that he's also experienced concussion.
Sports is not the root problem, so quitting them is not the answer, Gill insists.
Soccer earned her a scholarship and allowed her to become a first-generation college graduate, she says, adding that it also beat her up on occasion. She doesn't remember much about her worst collision with the goal post. But long before she thought about using sweat to diagnose TBI, her head injuries had stealthily activated certain biomarkers within her own brain.
Gill's personal experiences speak to the ubiquity of TBI. In fact, a stunning one in three people experiences jolts, collisions, and blows—on sports fields, battlefields, and highways, not to mention in homes—that rattle the brain enough to affect everything from cognition and balance to mood, sometimes for months and even years to come.
Tough to diagnose, TBI is even tougher to study. It presents differently across individuals, and people recover (or don't) in their own unique ways. Safeguarded by the skull and protected by the blood-brain barrier, the body's most complex organ is as secretive as any teenager about its goings-on.
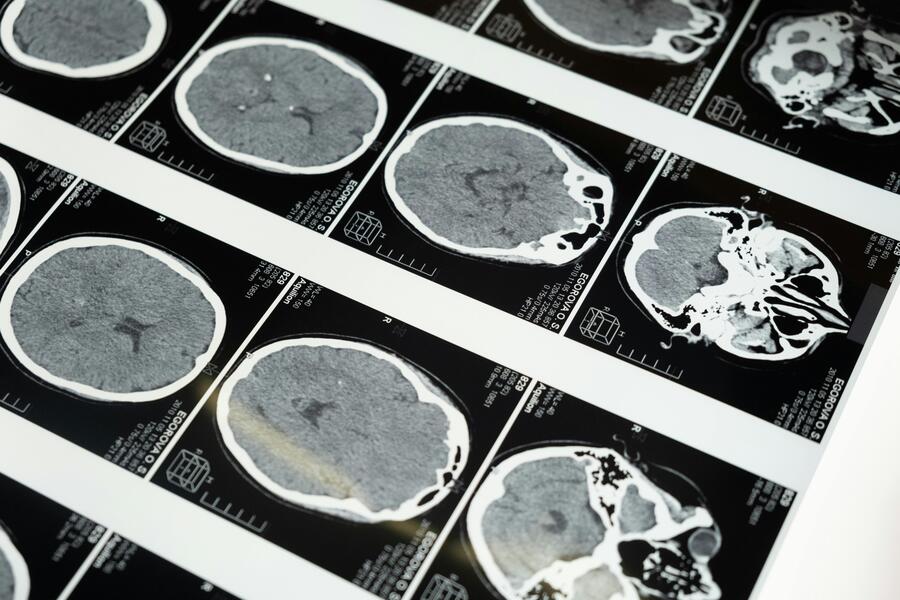
Although CT scans are important for determining whether someone needs a neurosurgical intervention after a head injury, a negative scan doesn't rule out TBI. In fact, of all CT scans given across the U.S., just 3% to 4% are positive, and of those, only a smattering indicates the need for surgery. Granted: CT can find those few devastating cases, Gill says, but it misses countless subtle injuries that also damage the brain.
Plus, CT is costly in terms of money and time. It's not unusual, as Gill knows all too well, to wait for 12 hours in an emergency department with a TBI, only to leave with a pounding headache and important questions that are more likely to elicit informed opinions from docs than definitive answers: Is it mild or severe? Am I allowed to sleep or just rest? When is it safe to return to work or play?
Gill, who spent decades studying TBI in military personnel, has since expanded her biomarker research to involve a wide range of populations. Now, she's kicking off a new study in collaboration with the Johns Hopkins football team that involves collecting sweat from players for the purpose of biomarker analyses.
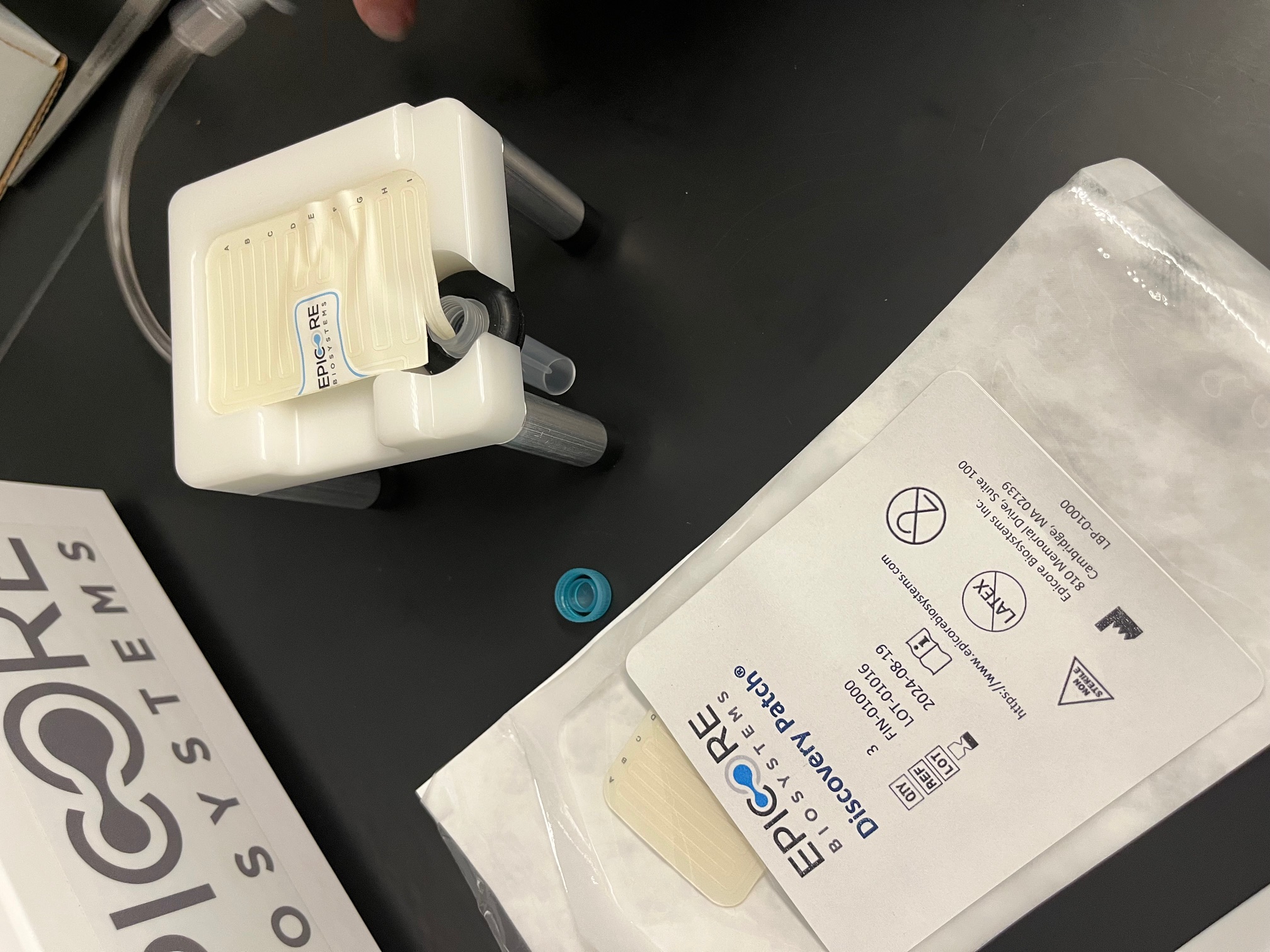
Image credit: Maryalice Yakutchik
Sweat, like blood, holds valuable clues about complex biological processes. But unlike blood, it's easy to get. Stockpiled in Gill's lab are noninvasive adhesive patches, destined for the upper abdomens of Blue Jays who agree to sweat for science. At the start of the season, players will wear the patches while running on treadmills for a primary collection to measure proteins at baseline. Subsequently, patches will be worn during play and sweat collected throughout the season for comparative analyses using OLINK. The big questions are: After a hit to the head, are any proteins— alone or in concert—different from how they appeared at baseline? Is one protein elevated, for instance, or is a group of proteins acting out of character? And does this relate to the recovery trajectory of the athlete?
Gill's long view is for collection and care to happen right away, when and where injuries occur. What transpires this fall on the Hopkins football field and in Gill's lab will be important steps toward the goal of designing a simple but refined test for TBI diagnosis and prognosis. As an analogy, Gill suggests thinking about how the protein biomarker troponin (in blood) allows doctors to distinguish between heart attacks and panic attacks, which can present similarly but require vastly different treatments. Ideally TBI biomarkers in sweat someday will allow an athletic trainer to diagnose and advise players about treatment and prognosis post-TBI.
Tyler Golembrosky, the Jays' head athletic trainer for football, looks forward to a time when return-to-play decisions are based on biomarkers and not subjective tests, much less the entreaties of overeager student athletes who, having had their brains injured—and perhaps having had decision-making and impulse control impacted—insist they are ready to get back into the game now.
Hey, Teddy Gill! Consider that fair warning. Or maybe a mother's promise.
Posted in Science+Technology
Tagged neuroscience, nursing, neurology, veterans, traumatic brain injury, sports injuries