The six first-year med students approach the table, the place where for the next seven weeks they'll spend so much time, it will seep into their dreams. They brace themselves to meet him. Him, their cadaver.
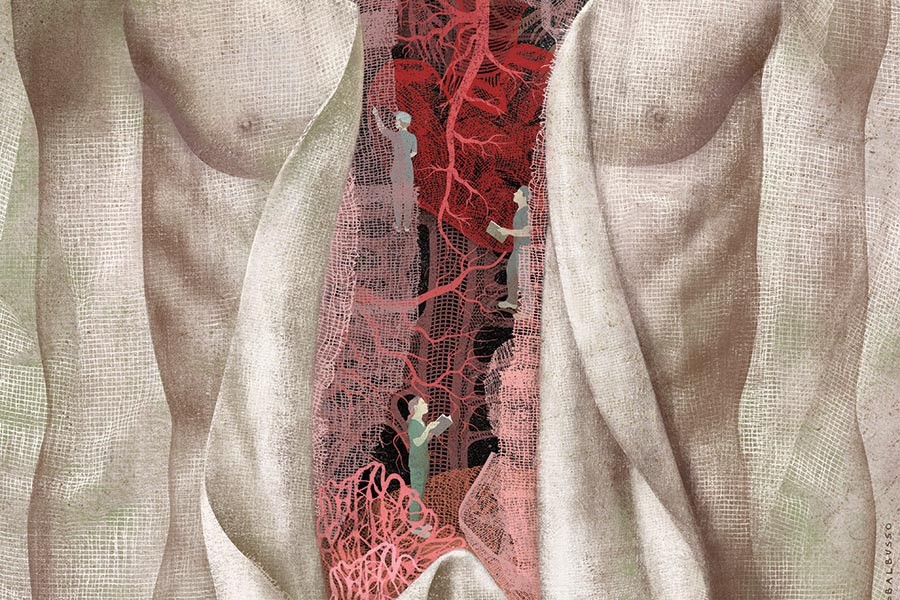
For some, even those who have lost a loved one, it's the closest they've ever been to a corpse. But soon enough, these students will spend their days inches away from this man's body, cutting through his skin, peeling back the fat, and trimming away the fascia—those bits of densely woven tissue that encase the body's innards—to see his stomach and liver and bones. Soon enough they'll pull on his tendons and watch as his toes wiggle in turn. They'll cut his digestive system from esophagus to rectum, making much ado about the smell. They'll hold his heart in their hands, and they'll saw open his skull to remove his brains.
These are the Johns Hopkins School of Medicine students of Table 4D: Sina Famenini, Sara Jones, Ravi Medikonda, Jeremy Applebaum, Nathan Yueh, and Jennifer Qin. One week into med school, they are handed their first patient. He'll teach them more about gross anatomy than they ever thought they could absorb in seven weeks. But he'll also teach them how to care. How to detach. How to work as a team. A sense of curiosity and discovery. How to navigate the emotions they'll face when they become fond of a patient but have to put him through the most painful experience of his life in order to make him well again.
They unzip the body bag and slowly peel back layers of plastic tarp and cloth to reveal his pallid, almost gray face. They decide to call him simply "him." For privacy reasons, they aren't told his name, and a nickname seems disrespectful, as if to minimize who he was when he was living. They thank him aloud for the gift he made to their medical education. Famenini grasps a scalpel, holds his breath, and makes the first cut.
As they work, the students move from Grant's Dissector, the book that guides them through the day's to-do list, to the cadaver, to a computer screen, back to the cadaver, trying to identify body parts and figure out what, and what not, to cut. Table 4D is tucked away in the last of four bays, each of which holds six dissection tables. Twenty-four bodies in total. Most of the 140 students in the lab are first-year med students, but there are a handful studying biomedical engineering and a few aspiring medical illustrators. A steady hum of conversation is occasionally interrupted by a brief commotion of discovery as the teams work just a few feet from one another.
Some cadavers have pillows of exposed fat while others, like 4D's, look emaciated.
Some are tall, some short, some black, some white. Some have lungs that show years of breathing in harsh chemicals. One, near the entrance, still has a bright pink manicure that looks as though it could have been done hours before death. Another is missing his left leg, with a bullet wedged into his skull. The bodies have all been embalmed, and the smell of formaldehyde lingers in the air despite the state-of-the-art ventilation system installed in the lab. Above each table hangs a light, much like the one a dentist uses to get a better view of your molars. Below is a pan that catches drippings from the body, such as preservatives or fat that has melted under the lamp; students will often reuse this "juice," as they call it, to keep the body moist.
Famenini, Medikonda, and Yueh are taking the first shift at the table while their tablemates attend a session on abdominal imaging. Their cadaver, an elderly man with age spots dotting his skin, lies on the table with a tarp covering his lower half. His chest is open, and his rib cage, sawed out a few days earlier, rests atop his face. As they fumble their way through his abdomen, there are a lot of comments like, "It should be there" and "I think this is it." They cut slowly and carefully—once something's been snipped, there's no going back.
"Is that the omentum, or is that … ?" Famenini trails off.
"This is part of the greater omentum," Yueh answers.
"So it goes over from the major curve—the anterior of the stomach folds down and up to the … small intestine," Famenini says.
"Actually, no," Yueh responds, "the greater—this is it. That's not greater omentum."
"Oh yeah. Might be lesser omentum," Famenini says.
"No, lesser is this," Yueh says, pointing.
The clock is ticking. By Friday, Famenini needs to know this information by heart (or, well, by stomach). It's his turn to give a rapid-fire 15-minute presentation, complete with Q&A, on everything they've dissected this week.
Today, med students have detailed medical atlases and 3-D visualization software that point out every muscle and nerve and bone. As technology advances, so do educational tools, with ever more realistic and advanced representations of the human body. But cadaver dissection remains an essential part of medical school education in the United States. Why is that? What do students get out of the experience that can't be had through software and hands-on patient experience?
Chris Ruff is the director of the Johns Hopkins Center for Functional Anatomy and Evolution. Like most who teach anatomy at Johns Hopkins, Ruff is an anthropologist, specializing in the evolution of human skeletal anatomy over the last 6 million years. It makes sense for anthropologists to teach the course, he says: Clinicians or retired surgeons, for example, have likely spent so many years specializing in one area of the human body that they won't be able to answer the broad range of questions students will have as they work. To incorporate those specialists' arsenal of expertise, students attend lectures and get hands-on demonstrations from clinicians on things like imaging or pathology.
For more than 30 years, Ruff has watched as students spend their first weeks of med school in the anatomy lab. He doesn't get sentimental about what the course represents—his goal is to ensure students leave armed with information more than a memorable experience—and winces when people call dissection a med school initiation or rite of passage. However, he acknowledges its significance. It's a once-in-a-lifetime experience shared by very few people, most of whom are in the same line of work. "There has been a tendency over the years for this to be seen as an initiation or something like that, something you have to get through," Ruff says. "And in a sense, it is. It is something that almost no one except medical people do, so you are kind of part of a club by having done it. But that's not the reason we're doing it. It's to learn something that you're going to use all the time, and that, at least in our opinion, you can't learn any other way as effectively. It just makes so much more of an impact. Even if people did almost as well on written tests by reading a book and looking at a computer, I don't think they'd be as good doctors without this experience."
When Maryland's medical schools need bodies, they call Ronn Wade, the director of the Maryland State Anatomy Board as well as of the Anatomical Services Division at the University of Maryland School of Medicine. Wade grew up in a family-owned funeral home, directs mortuary continuing education classes, is a licensed funeral director, co-directed a research project to replicate Egyptian mummification, and oversees the distribution of the state's bodies for medical research. Over the past four decades, he has simplified donor forms, changed and clarified laws, and publicized the option of body donation to people making end-of-life arrangements. Today, Maryland leads the nation in card-carrying body donors. "Maryland is a little bitty state," he says, "and for us to have about 80,000 people walking around with donor cards, that's a lot." The number of bodies that come to the Anatomy Board goes up 2 to 3 percent each year, he says. In fact, Maryland gets so many donors that the Anatomy Board often helps other states that have supply-and-demand issues.
The board gets its bodies in one of two ways: Either the person has filled out a short form willing his or her body to donation, or the deceased becomes a "donor by circumstance," as Wade calls it. In those cases, either the family could not be reached or they're unable to take custody of the body for financial or logistical reasons (they can't afford a funeral, or the family lives out of state, for example). After 72 hours, it legally becomes the responsibility of the board, an entity within the Maryland Department of Health and Mental Hygiene, to take control of the body. "The issue is, I have a person here who the paramedics could train on, that I have no pending claim on, that can help them learn to save people's lives," Wade says. "Or, I can hold off on it and the body's going to slowly decay away." It becomes a public health issue at that point, he says, so he opts to use the bodies in the way that does the most good.
When a body is bound for the Anatomy Board, the process goes something like this: If the person is an organ, eye, or tissue donor, the local organ procurement organization takes anything that could be used. Wade then gets a call and sends out a mortician to pick up the remains. It's brought back to the Anatomy Board, housed in the basement of the University of Maryland School of Medicine, where Wade and his crew look over the body to see if there's any evidence of HIV, hepatitis, tuberculosis, or other hazardous infection. If the body doesn't present any dangers, they decide how it can best be used. A body that is extremely heavy or tall, for example, makes a poor cadaver because it will be too cumbersome to move or might not fit on the dissection table. If a body has been ravaged by cancer, its anatomy will have been so altered it won't be a good teaching tool for med students. Likewise, if it has had several organs removed for donation. Those bodies can be used for other medical training—a plastic surgeon practicing a new technique or a paramedic learning to intubate—and can see up to eight to 10 uses each.
Of the 2,500 bodies that came to the board last year, just 400 were suitable for use as a cadaver, according to Wade. Those bodies were embalmed and then distributed to medical schools including the University of Maryland; Johns Hopkins University; and the Uniformed Services University of the Health Sciences in Bethesda, Maryland. Post-dissection, they are cremated, placed in neatly labeled black urns, and returned to Wade's office. If the family requested the ashes, they are returned. Otherwise, they go to the Anatomy Board's gravesite in Sykesville, Maryland, where a statewide memorial service is held each June. (Students at Johns Hopkins hold their own private memorial service after the course ends as well.)
Sometimes, Wade gets calls from the family members afterward. "People call. 'I just want to know what my mom was used for,'" he says. "And then I'll look on the calendar schedule and I'll see all the programs that are going on that she would have been in. I'll say, 'Let's see. We had an orthopedic program, we had plastic surgery, there was emergency medicine and paramedics.' And it's very comforting." Sometimes, he says, he gets to tell them that their loved one finally made it to med school.
In fall 2015, a few of the first-year students planning a memorial service for the cadavers proposed a more permanent monument at Johns Hopkins for those whose bodies are donated. They formed a student group named Hum-An, short for Humanistic Anatomy, and are working with School of Medicine leadership to create a memorial garden next to the building that houses the anatomy lab.
"It occurred to us that it's a very transient experience," says Anna Goddu, Hum-An co-chair, as she stands in the proposed space for the public garden on the lawn west of the Armstrong Medical Education Building. "The whole thing is this intense seven weeks where you spend hours a day with your cadaver, and then after seven weeks, all of a sudden they're just sort of gone. And the memorial service is a wonderful tribute, and I think an important one, but it's also just a moment. There's no real sort of permanent mark of this experience that opened your medical education, no recognition that over many years, there are generations of people who have contributed to our education in that way."
Hum-An collaborated with the school to install an 18-foot-wide labyrinth in the grass for walking and reflection. Two benches will seat a group of five or six, the typical size of each lab group. Wind chimes, a birdbath, and a plaque will go near an arbor. Hum-An members helped support this year's anatomy students, too, filling them in on what to expect, offering advice on how to get through the course, and passing on their memorial service plans. "This year, on the first day of Anatomy, as I was walking toward the building, I was like, There are 24 people in there," Goddu says. "Twenty-four extra people. I felt this extra presence in the building. There's this deep, deep sense of gratitude and amazement toward these people whose bodies were donated."
Midway through Anatomy, the students have started to trust their instincts more and divvy up the day's to-do list rather than watch nervously as one person applies scalpel to skin. The cadaver lies face down on the table, the skin removed from his legs to reveal atrophied muscles. The bits of skin and fat that speckle the table don't seem to faze anyone.
The students aren't given any information about their cadaver, so, for now, they invent their own. (They'll learn his age and cause of death on the last day.) "I like to think he was a family man, that he really took care of his family and worked hard," says Famenini. "There's no basis of me saying that, but that's just the feeling I get from this person." As he peels away the skin on the man's heel, which is now in stirrups, Famenini says, "We've been trying to think about what he did when he was alive. I'm thinking truck driver." "Or IT—a desk job," counters Medikonda. They wonder what kind of sedentary lifestyle could have been responsible for his poor muscle definition.
Wade says students become more intimate in some ways with their cadaver than his or her partner had been in life. They can look at a mailman's shoulder and see the wear and tear from carrying a heavy bag every day. They can even tell if the person was right- or left-handed. And yet, when students are bent over the table, 6 inches away from his leg, squeezing his nerves, veins, and arteries to try to differentiate each one, they're more concerned with anatomy than empathy. It takes seeing his hand or, as they learned, accidentally thumping his head while turning him over on the table, to snap that thought back into their minds. There's a constant back-and-forth. Zoom in, zoom out. Human being, teaching tool.
"It's important to remember that our cadaver was a living person at one time and had his own successes and failures and family and a personality and a life," Applebaum says. "That's very important to maintain when you're working with your cadaver because you want to show respect for their remains and recognize that the donation is one of the most important gifts they've ever given. You want to remember that it was a person and a patient. But when you're going through the dissection and proceeding through the body, it just feels very compartmentalized. We're looking at the legs and particular muscle structures without recognizing, 'Oh yeah, this is the leg of a person.' You get into the mindset of just having to work. You have your list of muscles and arteries and structures that you need to find, and you're so hyperfocused on that. And then there's a glimpse of the face or something, and you just stop and pause for a minute and remember what you're doing and why you're doing it, and it just becomes so much more important in that moment."
Some question whether cadaver dissection makes sense anymore. As schools push to incorporate more clinical experience earlier on, can't the same knowledge be gained from working with actual living patients? Isn't most day-to-day anatomy gleaned from medical imaging anyway? And with advances in technology, is dissection worth the time, money, and effort?
In 2004, the journal Anatomical Record invited faculty members from four medical schools to present their case. John C. McLachlan, then a professor at the Peninsula Medical School in the United Kingdom, argued that "modern 3-D reconstruction and imaging methods give views of the internal structures … that can be superior to those observed during dissection." He wrote that forgoing dissection in favor of clinical experience allows students to first encounter patient death in a much more natural setting and is less likely to cause desensitization. Another author, Kimberly S. Topp with the Department of Anatomy of the University of California, San Francisco, proposed prosection—professionally pre-dissected bodies—as an alternative to basic classroom dissections.
Technology advances make a cadaver-free medical education more possible with each passing year. In the 1990s, the National Library of Medicine's Visible Human Project created anatomical, three-dimensional representations of a murderer from Texas and a housewife from Maryland by slicing, scanning, and photographing cross sections of each body. In Korea and China, more recent versions of the U.S. project give even more detailed, higher-resolution images. In 2015, a scientist from Tampa went on the TV show Shark Tank to pitch to investors his $40,000 prototype of Syndaver, a synthetic human cadaver that mimics real human tissues and organs in not only appearance but feel. And Silicon Valley startup Anatomage has created products including the Anatomage Table, a life-size visualization tool that uses the images from Korea, among other sources, on an iPad-like display. Kris Thomson, director of applications for the Anatomage Table, says the $70,000 product is a bargain for smaller institutions, including community colleges and physical therapy or physician assistant programs. Instead of paying for a lab, ventilation system, prep fees, disposal fees, and so on, the schools can purchase the product one time and use it for years. For comparison, it cost $17,500 to operate the Johns Hopkins anatomy lab last year alone. Anatomage's products are also helpful for students who, say, have an allergic reaction to the chemicals used in embalming.
"I do feel like the technology is improving more and more each year," Thomson says. "I know our visual quality is leaps and bounds better than it was just a couple of years ago. I think more and more people are starting to recognize that and move away from just the cadaveric studies." Still, he says that while the Anatomage products, which also include a 3-D printed torso, can cover much of what students learn in conventional anatomy labs, there is still value to dissection. "It's hard to replace the feeling of being around an actual body, an actual person," he says. "It would be very difficult to have a virtual platform of any sort replace that feeling."
Ruff, who spends his mornings moving from table to table in the Johns Hopkins anatomy lab's first bay, reiterates that there's something about the hands-on process of dissection—the sense of discovering each organ's location for oneself, of identifying abnormalities in your specific cadaver's body—that can't be replicated. Diagrams in books or in a digital simulation can give you an idea of where things should be, but they're often idealized and oversimplified. The drawing might show the muscles or the bones or the cardiovascular system, but rarely will you see all of the above on one page. And it's nearly impossible to get the level of detail (or messiness) that you'll see in the flesh. They're helpful educational tools for reviewing systems after the fact. "But for really learning it and seeing it for the first time," he says, "it's like looking at a movie of someone hiking through the Grand Canyon versus actually hiking through the Grand Canyon.
"You don't get that three-dimensional feel. You don't get the texture, the variation, the reality of what bodies are like, without the cadaver. And also, just the process of finding things … it's very physical, very structural, geometric, spatial. You just don't get an appreciation for that otherwise."
Toward the end of the course, the cadaver's skin has been peeled from his face; the top of his head, cleanly sawed off, sits on the table as a dish for his brain. One of the last things students will have to do this week is disarticulate the head—chisel away at the spinal column to separate head from neck.
They're tired. When the students leave the lab most days, they grab lunch, then study until around 10 p.m., taking a brief break for dinner. They estimate that they spend 30 to 40 hours a week studying for this one course. Even now, as they're fastening colored paper clips to mark the arteries in the neck, they're quizzing each other for the final exam. The number of mnemonic devices the students repeat is dizzying; Tom, Dick, and Harry, for example, refers to the order of ankle tendons from anterior to posterior: tibialis posterior, flexor digitorum longus, flexor hallicus longus. Tom, Dick, and very nervous Harry takes it a step further to include artery, vein, and nerve. Every once in a while, someone goes to the whiteboard next to the body to draw a nerve structure.
Famenini thinks back to day one, when they were told the cadaver would be their first patient. "And it became a cliché and flew over my head. How could a cadaver be our first patient? I did feel that dichotomy of, How could going through someone's body in a very systematically violent way, kind of dismembering them, literally, how could that teach us empathy and understanding of a patient? However, as I've gone through and gained a much better appreciation of the complexity—the internal planning of the human body—I've kind of seen how different things have to all work together to work right, how things have to go wrong on the inside to give a patient pain or discomfort, or how some problems that could be summarized in one clinical term, like 'heart attack,' could have ramifications. It's definitely given me a deeper appreciation of the inner workings of the human body and how they all work together to make someone's life go on."
After the exam, the students will get a couple of pieces of information. Age: 93. Cause of death: vascular dementia and hypertension. They'll say goodbye to the lab and their cadaver. A few weeks later, they'll hold a memorial service, where they might sing songs or read poems. And then they'll move on to the next course, and the next one. But as they learn about the kidneys or the lungs or the heart, it's his they'll picture.
Posted in Health
Tagged anatomy, physiology, medical school, cadavers