It started with a bit of blood.
In April 2013, then 68-year-old John Ryan checked in with his primary care physician after he suddenly began to cough up trace amounts of blood. One emergency room trip and several tests later, the 30-year Navy veteran was told to prepare for his toughest battle yet: stage 4 non-small-cell lung cancer, adenocarcinoma.
"We weren't sure what was going to happen," says Ryan, a father of eight. "I was given 12 to 18 months to live if I started on chemotherapy immediately, and we knew time was valuable, but so much was unknown."
Ryan began a course of chemotherapy treatment soon after his diagnosis, but he suffered from debilitating side effects. When the pain, fatigue, and weight loss caused by the chemotherapy became too much for Ryan, he sought a second opinion, which brought him to Johns Hopkins Medicine and oncologist Julie Brahmer.
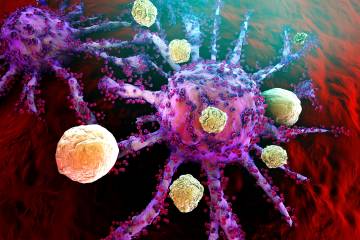
At the time, Brahmer was a principal investigator in a phase 3 clinical trial at Johns Hopkins Hospital for nivolumab, an immunotherapy known as an anti-PD1 drug. The trial built on years of National Cancer Institute-funded research at Johns Hopkins Medicine, including investigations into cancer immunology and the body's immune system. Ryan was added to Brahmer's trial and was randomized into the cohort receiving immunotherapy.
Within months of starting treatment, after only four nivolumab infusions, Ryan's tumor shrunk by 65%. Through patient advocacy efforts by Ryan and Brahmer, he remained on the immunotherapy for close to a decade, receiving nearly 150 infusions. Researchers like Brahmer are continuing to try to learn how long patients who benefit from this treatment need to remain on immunotherapy. The clinical trial Ryan was a part of also helped lead to nivolumab—and other PD-1 drugs—being approved to treat other cancers.
"Mr. Ryan's journey is inspiring to a lot of patients, and the work we need to do now is figure out why he did so well with immunotherapy for so long," says Brahmer, professor of oncology at the Johns Hopkins University School of Medicine and the Sidney Kimmel Comprehensive Cancer Center. "Over the past 15 years, we've gotten closer, and that's why federal funding for research is so important—it helps us do deep dives into characteristics of cancer and patients."
Although Ryan's cancer appeared stable, in 2022 he experienced a setback due to the immunotherapy that saved his life. Rather than solely targeting his cancer, his body's immune system turned on him and began attacking the healthy parts of his lungs.
In March 2022, Ryan was diagnosed with pneumonitis, a persistent inflammation of the lungs that causes severe scarring and decreased lung function. He was forced to cease his immunotherapy treatments and seek additional care.
Brahmer connected Ryan with pulmonologist Karthik Suresh, who has studied and treated pneumonitis for years. Much of Suresh's training and research on pneumonitis, including training on conducting clinical and translational studies, was also made possible through federal funding from the National Institutes of Health.
At the time, Suresh had just started a clinic specifically focused on pulmonary complications of new cancer therapies at Johns Hopkins Medicine. He took Ryan on as one of his first clinic patients, prescribing him a mix of treatments to subdue his lung inflammation and, he hoped, restore lung function.
"We crafted this new regimen of steroids and other medications for Mr. Ryan to treat his case, which was really severe, and our efforts to understand his disease were supported by robust research infrastructure," says Suresh, an associate professor of medicine at the Johns Hopkins University School of Medicine. "Our patients, like Mr. Ryan, are waiting for these types of treatments, for cures, and without investments into research, these won't be coming. Physician-scientist training relies on federal funding—without programs to train future scientists, none of this care would exist."
In 2025, Ryan was officially cured of his pneumonitis, a stark improvement from having just 28% lung function during the worst of his condition. His cancer remains stable, even after stopping immunotherapy due to its side effects. Despite his difficult diagnoses over the years, Ryan credits staying positive and staying knowledgeable about his conditions as major factors that gave him strength during his journey.
"Having trust and faith in what's happening is crucial when you're on the other end of the spear," Ryan emphasizes. "I would have been dead in 2014 had Johns Hopkins not taken the lead. And if it wasn't for sharp, capable researchers, like Dr. Brahmer and Dr. Suresh, I would've lost my life either from lung cancer or pneumonitis. I'm grateful to them, and all of the staff who cared for me."
Posted in Health
Tagged nih funding, lung cancer