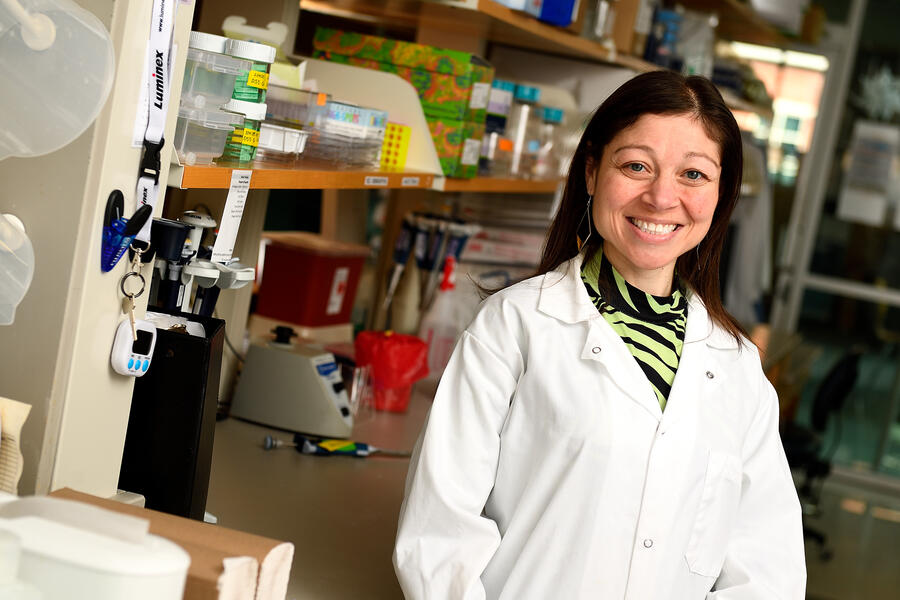
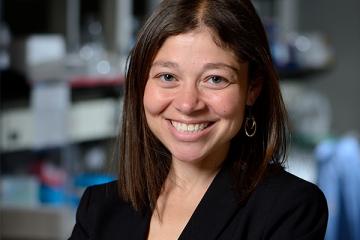
Jamie Spangler oversees a lab of 33 scientists at Johns Hopkins who are developing new, targeted treatments that harness the power of the immune system.
With the backing of the National Institutes of Health, Spangler and her team use the body's natural resources—its cytokines, antibodies, antigens, and T cells—to fight infectious diseases and cancer, as well as to stop or reverse the development of autoimmune disorders like multiple sclerosis, type 1 diabetes, rheumatoid arthritis, and colitis.
But "a cloud of uncertainty" hangs over the research community now amid threats to NIH funding, says Spangler, an associate professor in the Department of Biomedical Engineering and the Department of Chemical & Biomolecular Engineering at Johns Hopkins University's Whiting School of Engineering and School of Medicine.
"The NIH cuts have created tremendous anxiety," she says of a recent announcement by NIH that it planned to curtail its funding support for research by capping reimbursements for essential expenses known as indirect costs. "Indirect costs help keep the lights on in our lab, while paying for the administrative support, technology, and equipment it takes to do our work."
An award-winning scientist, Spangler and her team work at the forefront of immunoengineering, an emerging field that experts say is revolutionizing how complex diseases are treated. The lab uses an interdisciplinary approach at the interface of engineering, biology, and medicine to rewire the immune system in order to ward off disease. As Spangler puts it, "we use and manipulate molecules and proteins that exist in nature to reprogram aspects of our biology to intervene and reverse the disease process."
Funded in large part by the NIH, the work of Spangler and her lab along with their many collaborators has led to dozens of breakthroughs and discoveries, including:
- Reprogramming regulatory T cells to suppress the immune system and stop the onset of inflammatory bowel disease and diabetes
- Engineering proteins to prevent tumors from developing and progressing in cancer patients
- Engineering chimeric antigen receptors to enable the body's natural killer (NK) cells to fight acute myeloid leukemia
- Devising a fast, inexpensive way to detect SARS-CoV-2 (COVID-19) antibodies with commercial blood glucose monitors
Funding support for graduate students is vital, as "they're the backbone of research across the country, doing the bulk of the work and making valuable contributions every day," Spangler says.
The consequences of losing NIH funding, she says, could be detrimental to the millions of people in the United States and around the world who suffer from immune-related diseases, such as cancer and autoimmune disorders. Cancer incidence continues to rise, and in the U.S. alone, approximately 50 million people live with one or more autoimmune diseases, with the numbers increasing at an alarming rate. For instance, the number of adults living with type 1 diabetes nearly doubled in the past 40 years, while rates of multiple sclerosis rose roughly 30% over the past decade.
"Research is the lifeblood of the advancement of society, allowing us to understand and navigate the world in which we live," Spangler says. "It's critical to understand the catastrophic consequences these cuts can bring, not just to [our lab] but to the health and advancement of humanity—and to the standing of the United States as a global leader in medical research and innovation.
"All of that is at stake."
Posted in Health, Science+Technology
Tagged nih funding, autoimmune disease