Hearing loss is an inevitable aspect of aging. Everyone experiences it to some degree. But for more than a third of those age 65 or older, the loss is severe enough to be an impairment. And our aging population means hearing loss rates are rising, projected to double by 2060.
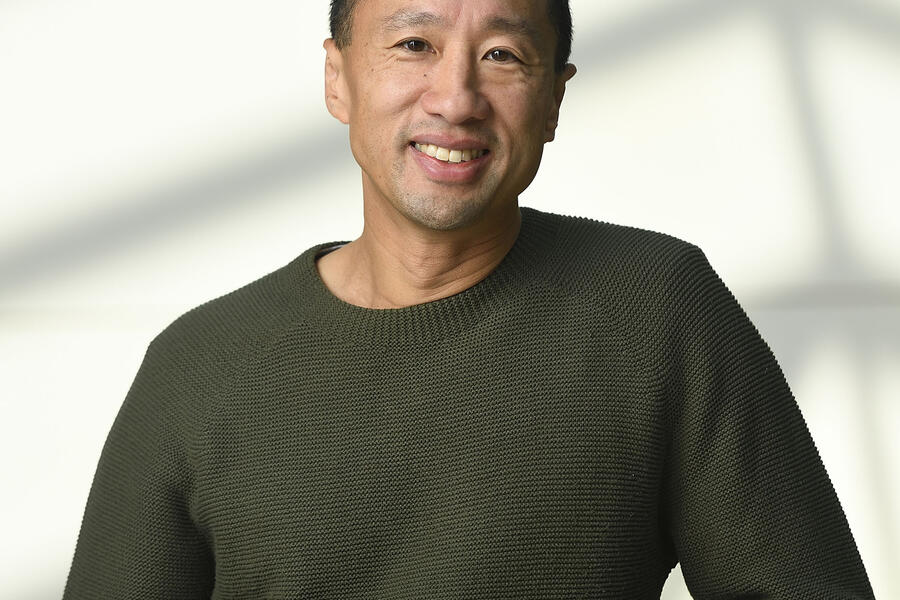
Frank Lin, director of the Cochlear Center for Hearing and Public Health and a professor in the Johns Hopkins University School of Medicine, has spent the past 15 years studying the broader health implications of hearing loss, fueled by more than $20 million in NIH funding. Hearing impairment in older adults is far more than just a quality-of-life inconvenience. It is associated with greater risk for dementia, cognitive decline, memory problems, decreases in brain mass, and depression.
"What the NIH funding did was lay out the evidentiary base for why hearing is important," Lin says. "If you don't have that evidence, you can't gain traction for the policy changes needed to address the issue."
Lin's latest ongoing NIH project is called Aging and Cognitive Health Evaluation in Elders, or ACHIEVE, a study to determine if hearing aids can address the myriad health issues related to hearing loss. The primary results show that for older adults at increased risk for cognitive decline, hearing intervention slowed down loss of thinking and memory abilities by 48% over three years. "We developed the first [randomized] trial ever to show demonstratively that treating hearing loss actually reduces things like cognitive decline," Lin says. "Does treating hearing loss actually make a difference in someone's life? You bet it does."
To increase the use of hearing aids among those poised to benefit from them, Lin swapped his scientist hat for a policymaker's. He worked with the National Academy of Medicine on policy language that became the 2017 Over-the-Counter Hearing Aid Act, which President Donald Trump signed into law during his first term with broad bipartisan support. Prior to this act, hearing aids had to fitted by a licensed audiologist, which made them more expensive and time consuming to acquire. The moribund hearing aid market had little competition or incentive to innovate. The act created a class of hearing aids that can be sold over the counter, like the way farsighted folks can conveniently pick up reading glasses from a rack at the drugstore. New high-tech makers have entered the hearing aid market, making devices that are both better and cheaper, while FDA oversight of the devices assures consumers of their safety and effectiveness.
"The average cost of hearing aids several years ago was like $4,700," Lin says. "Apple entered the market three months ago and a pair of AirPod Pros are something like 200 bucks."
Hearing impaired consumers can now save their brains from a range of debilitations while saving money in the bargain. All the result of NIH funding creating the bedrock of evidence required to drive change.
"Like many systems, NIH grantmaking could be made more efficient," Lin acknowledges. "But this partnership between the federal government and academic institutions to support American science has reaped untold rewards. You don't see the same level of science support anywhere in the world. Our institutions are where everyone around the world wants to come to do science because of the financial security and knowledge that the resource will be there year in year out."
Posted in Health
Tagged nih funding, hearing loss