I am a cancer researcher and a cancer survivor.
A few nights ago, I came across a post on X by @NIH that (seemingly) proudly announced massive cuts to the indirect cost rate on all current and future grants. My immediate reaction was to mutter to my husband, "Oh my God, I might lose my lab." My next thought: As a cancer patient, I am frankly terrified of the potential consequences of halting biomedical research.
For 20-plus years now, I have been working to figure out what causes prostate cancer. It is 2025, and we still do not know what causes the most commonly diagnosed cancer in males in the United States. This is not an easy puzzle to solve, but our work along with other research groups has gotten us so close to defining what puts people at risk.
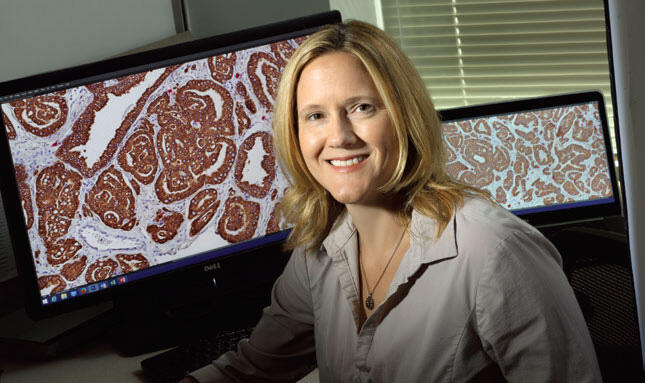
Image caption: Karen Sfanos studies the cellular and molecular pathology of prostate cancer.
We are working to determine why prostate cancer is fatal in some people and not in others while pursuing a new line of research to understand how the human microbiome—the trillions of microorganisms that live in and on our bodies—influences prostate cancer treatment response. The discoveries that we have made in the laboratory have led directly to a clinical trial that is slated to open this month.
To pursue this work, I was awarded my first "R01"—a five-year NIH grant that serves as the lifeblood of many research labs. The NIH funds research that directly leads to the development of new cancer treatments, and to clinical trials that inform clinicians on how to treat people with cancer. Cuts to the NIH's ability to fund biomedical research are intrinsically detrimental to people living with cancer, especially at a time when there is an alarming trend in increased incidence of many types of cancer, particularly in younger individuals.
Indirect costs help to provide the infrastructure for conducting biomedical research, and that is an exceptionally expensive undertaking for large research-oriented universities such as Johns Hopkins. It is entirely possible that indirect cost rates are due for reform at some institutions, but immediate, deep cuts to these funds mean that biomedical research across the country is suddenly in jeopardy.
The NIH funding cuts coincide with a saddening trend in the public's perspective and understanding of what researchers do, as well as an overall mistrust in scientific research.
NIH-funded clinical trials informed the treatment that I received after my cancer diagnosis. NIH-funded research and clinical trials are likewise critical to the continued development of treatments for people whose cancer has recurred. We cannot risk jeopardizing ongoing research progress in laboratories across the country—there are too many people suffering from cancer and too many lives at stake.
Karen Sfanos is a professor of pathology, oncology, and urology at the Johns Hopkins University School of Medicine whose research focuses on the cellular and molecular pathology of prostate cancer. She is also among the inaugural cohort of the university's Provost's Fellows for Public Engagement, a group of scholars selected to take part in a yearlong program designed to build their public engagement skills across a range of platforms and audiences.
Posted in Voices+Opinion











