PeriCor, a company co-founded by mechanical engineering PhD student Justin Opfermann, has been awarded a Phase II Small Business Innovation Research grant from the National Institutes of Health.
Totaling $1.8 million over two years, the funding will help the company to pursue the commercialization of PeriPath, a tool that will allow clinicians to implant cardiac devices in pediatric patients without the need for open-chest surgery.
Infants and children who suffer from heart arrhythmias may require implantation of a cardiovascular implantable electronic device, or CIED, such as a pacemaker or defibrillator to help control their heartbeat. Currently, the standard for CIED implantation requires the surgeon to cut open the patient's ribs, exposing the heart, so that a pacemaker's wires can be sutured to the heart's exterior.
Recovery from the surgery can be very painful, and requires the child to remain in the intensive care unit for several days. The surgery also creates adhesions—scar-like tissue—which increase morbidity and make future surgeries more challenging.
"Pacemaker wires are only about one millimeter in diameter. It doesn't make sense that a surgeon should have to cut open a child's chest to sew on something so small. We thought there must be a minimally invasive alternative," Opfermann said.
Prior to joining Johns Hopkins in 2020, Opfermann was a project manager and senior research and design engineer at the Sheikh Zayed Institute for Pediatric Surgical Innovation at Children's National Hospital in Washington, D.C. It was there that he and collaborators first developed PeriPath.
The plastic multi-channel tool gives the doctor access to the heart through a small single incision, allowing pacemaker wires and equipment to be inserted underneath the patient's ribs, instead of through them, as is done in open chest surgery. The device also includes a small camera so that vital cardiac structures can be observed and avoided during the pacemaker surgery.
"You can implant pacemaker and defibrillator leads through a single incision, smaller than a dime," Opfermann said. "By eliminating the need for open chest surgery, PeriPath reduces pain, decreases procedure time, and minimizes operative complications."
The highly competitive SBIR grant program provides support to early stage small businesses so they can bring scientific innovations from bench to bedside. PeriPath has already been tested and validated in animal trials, but the next step is to get approval from the U.S. Food and Drug Administration so the tool can be used in a clinical trial with pediatric patients. "The SBIR funding will streamline this process and help bring the PeriPath tool to market so more children can benefit from a minimally invasive procedure," said Opfermann.
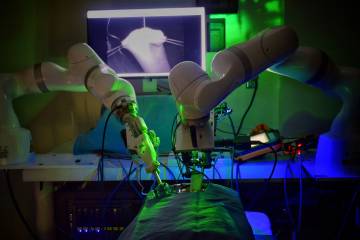
In addition to serving as chief operating officer of PeriCor, Opfermann will continue to work on developing novel surgical tools as a part-time PhD student in the lab of Axel Krieger, assistant professor of mechanical engineering and director of the Intelligent Medical Robotic Systems and Equipment Lab.
According to Opfermann, the SBIR award gives him and other researchers the best opportunity to make innovations such as PeriPath commercially available, which is not always an easy feat.
"This will provide a pathway to testing and studies that would otherwise be very challenging to do without major funding," Opfermann said. "It's very exciting to be able to translate a research idea into an actual product that can be used to improve patient outcomes."
Posted in Health, Science+Technology
Tagged graduate research