This article originally appeared in Johns Hopkins Medicine's Dome.
Ronald R. Peterson knows how many inpatients were treated on an average day in 1982 at Baltimore City Hospitals, which became Johns Hopkins Bayview Medical Center (about 500). He can tell you the budgeted operating expenses for The Johns Hopkins Hospital in fiscal year 2013 (about $1.8 billion).
Ask him almost anything about Johns Hopkins' administration and operations during the past 40 years, and he'll produce the answer.
Mastery of such detail is one of Peterson's astonishing abilities. So is his skill at working amiably with colleagues in every division within the vast Johns Hopkins Medicine enterprise, and so too is his sensitivity to patient needs and Johns Hopkins' role in the communities it serves.
These qualities help explain why he has steadily risen to ever more important positions of responsibility during his 44 years with Johns Hopkins Medicine—from increasingly critical administrative positions, to president of Bayview Medical Center, to president of The Johns Hopkins Hospital, to president of the Johns Hopkins Health System, to executive vice president of Johns Hopkins Medicine. These qualities also explain why he is so widely admired.
Although he will continue to serve as a special adviser to Dean and CEO Paul B. Rothman for at least a year, Peterson's retirement in January marks the end of an era at Johns Hopkins. It also highlights a career with few equals in the history of American health care systems.
Between meetings, over a lunch of no-salt vegetable soup and broiled salmon prepared in the hospital's cafeteria, the slim, bespectacled 69-year-old recently reflected on his role in many of the significant developments at Johns Hopkins Medicine during his more than four decades of service. This is his account:
1970s: Learning on the job
Peterson views the 1970s as his "learning period," the time in which he became the protégé of Robert Heyssel, director of The Johns Hopkins Hospital, a title that later became president.
A native of Edison, New Jersey, Peterson came to Johns Hopkins University as a premed student, hoping to become a physician. When he graduated in 1970, however, family circumstances compelled him to get a job rather than pursue a medical education. After working as a city school science teacher and as a part-time employee of a local kosher caterer, Peterson entered a George Washington University graduate program in health care administration in 1972. When the master's program gave him the opportunity for an administrative residency at The Johns Hopkins Hospital in 1973, he jumped at the chance—and never left.
Peterson recalls that Heyssel "sort of took me under his wing. ... He taught me to think strategically and to not be afraid to think a little bit outside the box." The hospital director also provided opportunities to tackle problems that went "a little bit beyond my own comfort zone."
Before Peterson completed his one-year residency, for instance, Heyssel sent him to work out administrative and financial difficulties at the hospital's Phipps Psychiatric Clinic—what Peterson calls "my first real job." Following his success at that assignment, the director asked him to devise plans for overall hospital cost-cutting measures.
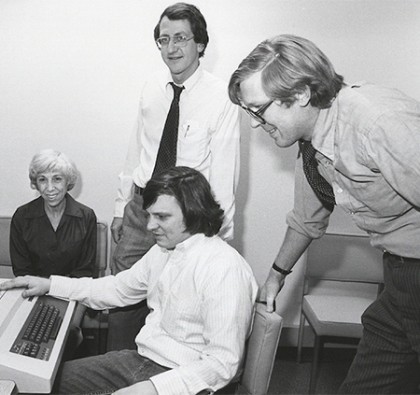
Image caption: Ron Peterson and fellow administrators discuss the hospital’s cost improvement program in 1976.
Incredibly, The Johns Hopkins Hospital had operated in the red throughout its first eight decades. Due to its commitment to the founder's mandate that his hospital care for those who could not pay, the hospital lost money from the day it opened in 1889. When Heyssel became head of the hospital in 1972, it was running a $1.2 million annual deficit. Under the cost improvement program that Peterson implemented, however, the hospital was operating in the black by 1977.
In 1978, Peterson's next challenge became righting the fiscal ship of the Children's Medical and Surgical Center, a 200-bed facility that offered various medical and surgical disciplines as well as subspecialties.
"I began to get the feel for actually running something, administering a hospital," Peterson notes. That experience—and the administrative adeptness it instilled—would prove invaluable when Heyssel gave Peterson his next big job: rescuing Baltimore City Hospitals and transforming it into what now is the Johns Hopkins Bayview Medical Center.
1980s: The once-in-a-career opportunity
Tracing its history back to the founding of the Baltimore City and County Almshouse of 1773, Baltimore City Hospitals was a storied municipal institution with an inspiring reputation for medical firsts—including the invention of landmark cardiopulmonary resuscitation techniques and the creation of the country's first intensive care unit. It was called Baltimore City Hospitals because it had both an acute general hospital and a chronic hospital that included a nursing home.
In addition, it had an association with The Johns Hopkins Hospital that even predated the opening of the university's School of Medicine in 1893. Many of its physicians held Johns Hopkins faculty appointments, and Johns Hopkins medical students long had done some training there.
By the early 1980s, however, City Hospitals staggered under annual losses topping $7 million to $8 million. Baltimore's mayor, William Donald Schaefer, wanted to unload it. Not only had running a major hospital become too complex for city officials; it was also causing a major hemorrhage in the city's treasury. Schaefer initiated the equivalent of a "request for proposal" for hospital organizations to take over its management.
Although a number of for-profit health care organizations offered proposals, the mayor was concerned they would "not take care of the poor people or do a certain service that was not making money," Peterson recalls. "Schaefer wanted assurance that whoever was going to run it would continue to care for all who needed access. So that's why I think they gave us the nod."
Heyssel believed that if Johns Hopkins could manage City Hospitals for a trial period and reduce its mammoth deficits, acquiring it would make sense. In 1982, he chose Peterson to head the group of Johns Hopkins managers who collaborated with City Hospitals' physician leaders to turn around the beleaguered medical center.
Under contract with the city, Peterson and his colleagues cut City Hospitals' losses by more than $7 million in just one year. By 1984, a joint committee of trustees from Johns Hopkins University and The Johns Hopkins Hospital accepted Peterson's recommendation that Johns Hopkins acquire the facility. Peterson was appointed president of what initially was renamed the Francis Scott Key Medical Center, and later named Johns Hopkins Bayview.
Peterson and his colleagues launched more than two decades of extensive, financially successful expansions of buildings, staff, and services. He says his work at Bayview stands as one of his finest achievements.
"To have been part of it was a once-in-a-career opportunity," he says. "It was a win for the city of Baltimore—no more red ink; a win for Johns Hopkins—130 acres of land on which to expand every dimension of our tripartite mission; and a win for the community, with dramatically improved facilities and services provided by Johns Hopkins faculty and highly competent, caring staff."
1990s: The creation of Johns Hopkins Medicine
When Peterson's mentor, Robert Heyssel, retired from the presidency of The Johns Hopkins Hospital and Health System in 1992, Peterson interviewed for his job.
Instead, the trustees hired James Block, a pediatrician from University Hospitals Clinic at Cleveland's Case Western Reserve University. They were concerned about what they believed was an increasingly competitive threat in the emerging area of managed care, and they considered Block to be especially well-versed in that field.

Image caption: "I have never worked with someone who has the work ethic, the unwavering moral compass to do what is right, and the ability to always treat everyone with respect that Ron Peterson has,” said Edward D. Miller (right), who served as dean and CEO of Johns Hopkins Medicine from 1996–2012.
However, the hiring of Block ushered in an extremely tumultuous time in the history of Johns Hopkins. Peterson recalls that the new president soon was "constantly knocking heads" with Michael Johns, dean of the School of Medicine, and sought Peterson's help with handling the situation.
"Block said he needed somebody to come and work with him who not only knew the organization but was recognized as a stabilizing force," Peterson says.
Peterson became executive vice president and chief operating officer for both The Johns Hopkins Hospital and health system, which then consisted of The Johns Hopkins Hospital, Hopkins Bayview, and the Wyman Park Health System, which included the then U.S. Public Health Service Hospital on the edge of the university's Homewood campus and the North Charles General Hospital. He also retained the presidency of Johns Hopkins Bayview.
The recruitment of Peterson as a "stabilizing force" didn't end the problems between Block and Johns. The medical school dean left Johns Hopkins to become executive vice president of Emory University's medical center in 1996. Block also departed that year.
Edward D. Miller, head of the Department of Anesthesiology, became interim dean, and Peterson was named interim president of both the hospital and the health system—while still remaining president of Johns Hopkins Bayview.
In 1997, Johns Hopkins Medicine was established as a unified leadership entity for the hospital and health system. Miller accepted the position of dean/chief executive officer, who would lead both the School of Medicine and the overall health system, as well as be the university's vice president for medicine. Peterson became president of the hospital and health system. Miller also named him executive vice president of Johns Hopkins Medicine.
Peterson and Miller formed a remarkable partnership. They not only solidified an effective governance structure for Johns Hopkins Medicine, but also led an equally dedicated team of administrators and faculty members to undertake extensive development projects and expand Johns Hopkins Medicine's scope dramatically over the next 16 years until Miller's retirement.
"We began to establish certain central services, began to do budgeting and planning on a consolidated basis. We began to speak with one voice in Annapolis and in Washington," Peterson recalls. "We began to develop the trappings of a 'system,' if you will. We created the infrastructure to do managed care with Johns Hopkins HealthCare. We began to develop the early stages of a home health services company to serve both adults and children."
In early 1998, Johns Hopkins Medicine acquired Howard County General Hospital, "with an eye toward thinking that we needed to begin moving outside of Baltimore and heading toward Washington," Peterson recalls. And the following year, he and Miller started to develop a physical master plan for the East Baltimore campus.
2000-2017: Building a new Johns Hopkins Hospital and a Regional Health Care System
Peterson considers the 2012 opening of the 1.6-million-square-foot Sheikh Zayed Cardiovascular and Critical Care Tower and The Charlotte R. Bloomberg Children's Center as a landmark achievement in his career.
"I take pride in having been able, on my watch, to do what was necessary to bring the physical facilities of The Johns Hopkins Hospital up to snuff, with excellent programs and people. From a tangible, physical evidence basis, that was especially meaningful. It remains a very visible sign of what we were able to accomplish," he says.

Image caption: “[Ron Peterson] is driven by a true caring for our patients, our employees and our local community,” said Redonda Miller (right), president of The Johns Hopkins Hospital, pictured along with Peterson (center) and Paul Rothman.
Peterson is also grateful that he could work with Miller and his successor, Paul B. Rothman, to develop "a more highly academically driven, integrated health care delivery system in the Baltimore-Washington region."
In 2006, Johns Hopkins Medicine entered into an agreement with the University of Maryland to jointly own and operate the Mt. Washington Pediatric Hospital in Northwest Baltimore. In 2007, Johns Hopkins signed affiliation agreements with the Annapolis-based Anne Arundel Health System, parent organization of the 370-bed Anne Arundel Medical Center; and the Greater Baltimore Medical Center, a 232-bed acute care hospital in Baltimore County.
In 2009, Johns Hopkins Medicine assumed control of the Suburban Hospital Healthcare System and its 230-bed Suburban Hospital in Montgomery County. Less than a year later, Sibley Memorial Hospital, a highly regarded, 342-bed facility in Northwest Washington, D.C., joined Johns Hopkins Medicine.
All Children's Hospital in St. Petersburg, Florida, had just opened a $400 million, 259-bed medical center in 2011 when it became the first Johns Hopkins affiliate outside of the Baltimore-Washington area. Since then, All Children's has been renamed Johns Hopkins All Children's Hospital and is in the midst of building a major research and education facility. The hospital's first class of residents graduated this year.
Johns Hopkins Medicine International has also experienced astonishing growth in the 21st century, with academic and clinical collaborations with hospitals, institutes, and clinics in Canada, Latin America, Europe, Asia, and the Middle East. Peterson participated in the creation of a major joint venture with Saudi Aramco, a global energy and chemicals company in Saudi Arabia. Johns Hopkins Aramco Healthcare collaborates with Saudi Aramco to provide care for approximately 360,000 employees, dependents, and retirees.
'Very Much a Hopkins Person'
Peterson says a key reason he has remained at Johns Hopkins for 44 years is because he "enjoys the people dimension"–interacting not only with his colleagues but also with patients and families. He routinely drops in unannounced at patients' bedsides, just to ask how they are faring and to offer a business card with the suggestion to contact him at any time.
"It's a way of keeping in touch with why I went into this business in the first place," he says.
Another reason he has stayed at Johns Hopkins is that the opportunities have outweighed the disappointments. When he was passed over for the jobs of the hospital and health system presidencies in 1992, for instance, he was soon traveling back and forth between East Baltimore and Bayview, juggling his role as Bayview's president with his new position as Johns Hopkins' hospital and health system executive vice president and chief operating officer.
Because of his many successes at Johns Hopkins, Peterson says, it has been easy to resist various outside job offers.
"A few were interesting, but I was always still very much a Hopkins person," he says. "I've had enough opportunity along the way to take on new, exciting responsibilities that have always provided me with a sense of renewal."
During his 20 years as president of The Johns Hopkins Hospital, U.S. News & World Report named it the No. 1 hospital in the nation 16 times, including 15 years in a row. Like Ron Peterson's service to the institution, it's a record unlikely to be matched.
Posted in University News
Tagged johns hopkins hospital









