Results of an initial study of tumors from patients with certain cancers shed light on the widespread acquired resistance to immunotherapy drugs known as checkpoint inhibitors.
The study, conducted by researchers on five patients at the Johns Hopkins Kimmel Cancer Center, suggests the resistance is due to the elimination of certain genetic mutations that enable the immune system to recognize and attack malignant cells. The results of their researcher is described online in Cancer Discovery.
"Checkpoint inhibitors are one of the most exciting recent advances for cancers, but the mechanism by which most patients become resistant to these therapies has been a mystery," says Victor E. Velculescu, program leader in the Bloomberg–Kimmel Institute for Cancer Immunotherapy at Johns Hopkins and professor of oncology.
Checkpoint inhibitors help the immune system recognize cancer cells by revealing evidence of mutated proteins called neoantigens on the surface of cancer cells. Clinical trials have shown that nearly half of patients with lung cancers eventually develop resistance to this class of drugs for reasons that have been unclear.
To investigate why checkpoint inhibitors so often stop working, Velculescu joined Valsamo Anagnostou, instructor of oncology at the Johns Hopkins University School of Medicine; Kellie N. Smith, a cancer immunology research associate at the Johns Hopkins University School of Medicine; and their colleagues at the Bloomberg–Kimmel Institute for Cancer Immunotherapy.
The team studied tumors of four patients with non-small cell lung cancer and one patient with head and neck cancer who developed resistance to two different checkpoint inhibitors: a drug called nivolumab that can be used alone or in combination with the second drug, ipilimumab.
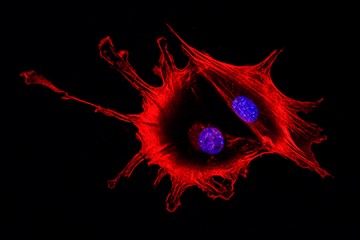
Using biopsies of the patients' tumors collected before the start of treatment and at the time patients developed resistance, the researchers performed large-scale genomic analyses to search for mutations specific to the cancer cells in all of each patient's 20,000 genes.
The search uncovered genes that code for the production of antigens, which serve as a source of identification to the immune system. Cancer cells may contain mutations in genes that code for antigens, producing misshapen or otherwise altered antigens that scientists call neoantigens. Such neoantigens are foreign to the immune system, and thus, the cancer cell is flagged for destruction, usually with the help of immunotherapy drugs.
The scientists found that after the patients developed resistance to immunotherapy, all of their tumors had shed between seven and 18 mutations in neoantigen-coding genes. By getting rid of those mutations, the tumor cells' neoantigens look less foreign to the immune system and may go unrecognized, say the scientists.
The researchers found that the tumors had lost these mutations by various means, including immune-mediated elimination of cancer cells containing these mutations, leaving behind cancer cells without the mutations, or by deleting large regions of their chromosomes in all cancer cells.
"In some instances," says Anagnostou, "we found that chromosomes in the cancer cells' nuclei were missing an entire arm containing these mutated genes."
Between one and six of the eliminated neoantigens were shown to generate a specific immune cell response in each of the patients, researchers found.
"Our findings offer evidence about how cancer cells evolve during immunotherapy," Velculescu says. "When the cancer cells shed these mutations, they discard the evidence that would normally lead them to be recognized by the body's protective immune cells."
Posted in Health, Science+Technology
Tagged cancer, johns hopkins kimmel cancer center, immunotherapy, bloomberg-kimmel institute